Article not found
This article is no longer available. But don't worry—we've gathered other articles that discuss the same topic.
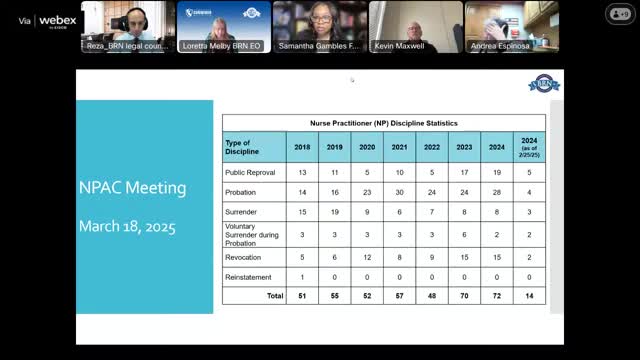
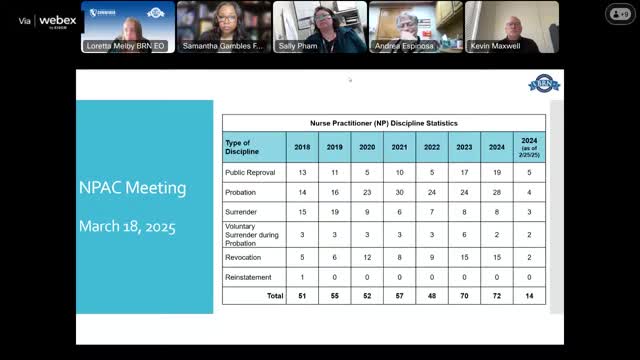
BRN advisory committee reviews SB1451 changes that expand 103 nurse practitioner practice and clarify retired certifications
BRN moves to ease out‑of‑state preceptor requirements; committee approves administrative motions including support for subcommittee scheduling
BRN posts proposed regulatory text and updates FAQs to implement SB1451; public comment period open