Article not found
This article is no longer available. But don't worry—we've gathered other articles that discuss the same topic.

House panel places omnibus higher education budget bill on general register after bipartisan compromise to shore up state grant program
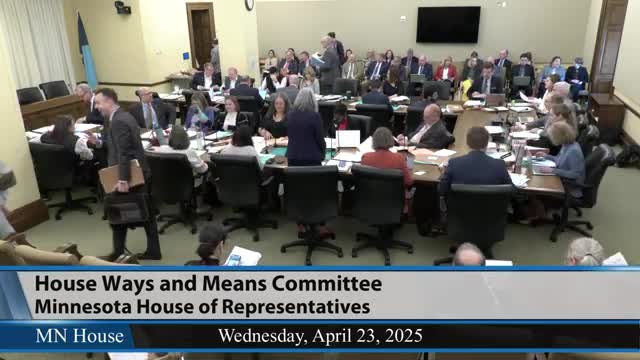
Committee lays over omnibus state government finance bill after adopting technical revenue and drafting corrections

