Article not found
This article is no longer available. But don't worry—we've gathered other articles that discuss the same topic.
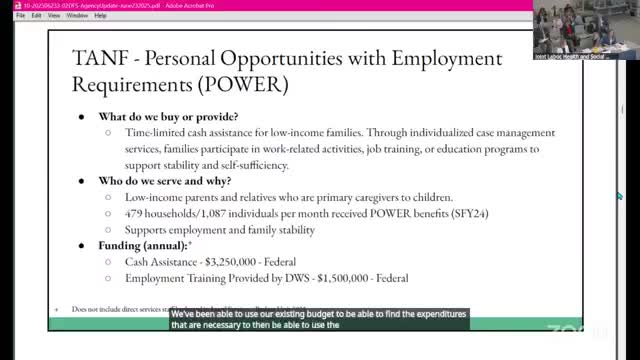
Department of Family Services briefs committee on TANF, SNAP, energy assistance and child support; SNAP-waiver questions surface
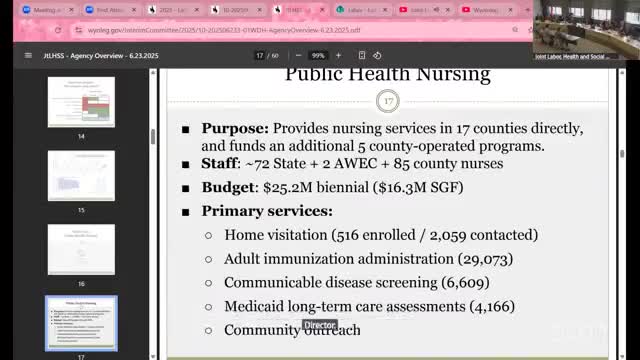
Department of Health highlights public health services, lab work and early signs of declining suicide trend
Department of Health briefs committee on Medicaid enrollment, budget and eligibility rules
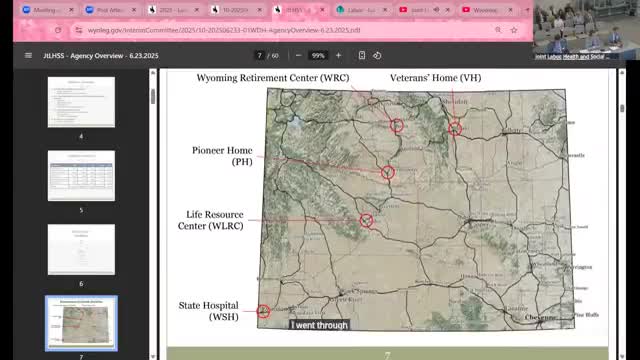
Wyoming Department of Health describes staffing shortages at state care facilities, heavy reliance on contract labor