Article not found
This article is no longer available. But don't worry—we've gathered other articles that discuss the same topic.
How Cardinal Care plans say members can access benefits, get help finding providers and use dental/vision services
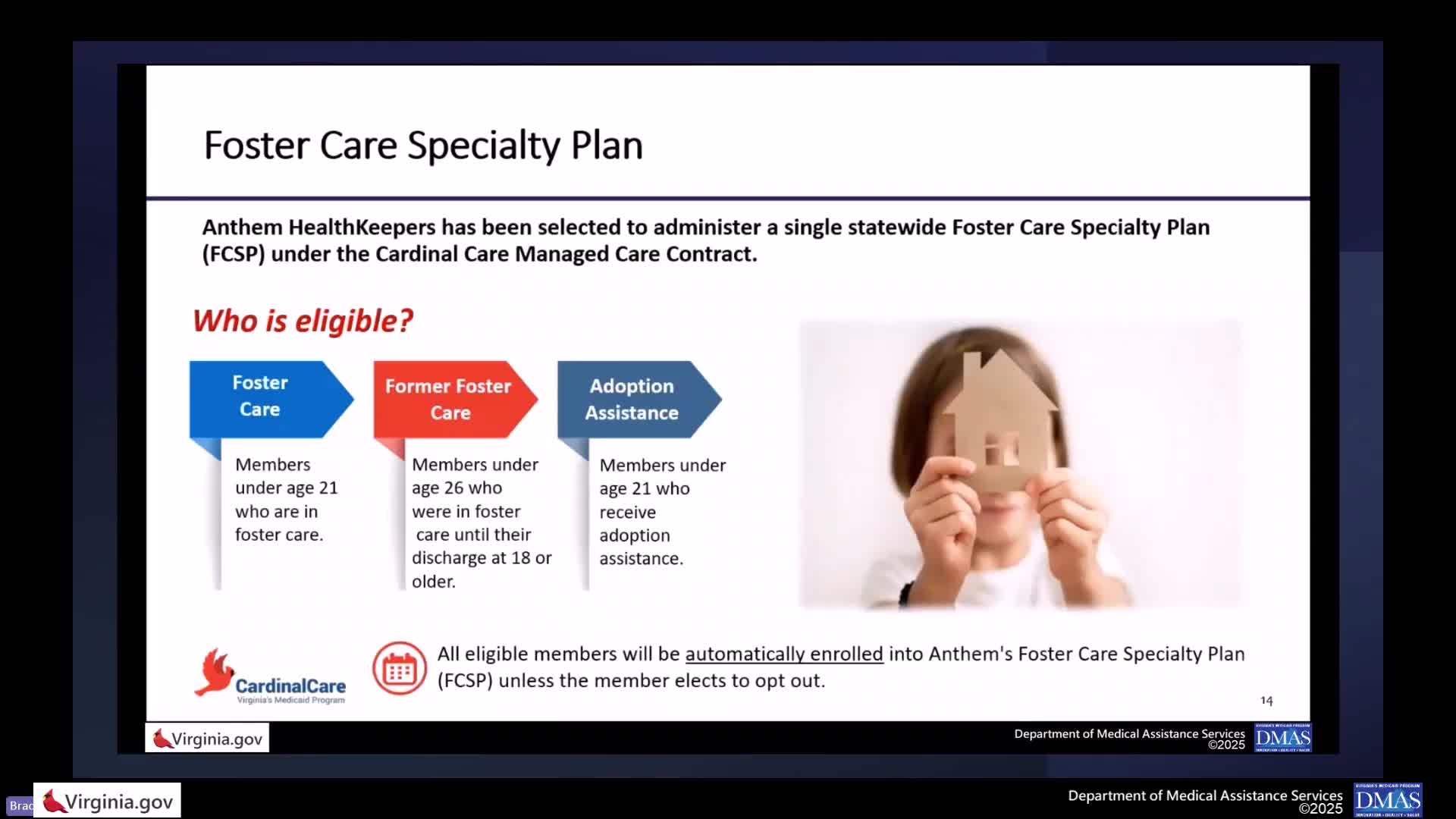
Anthem to administer Cardinal Care foster‑care specialty plan; dedicated supports and enrollment timeline previewed