Connecticut nursing‑home occupancy edges up to 89.2% as state panel discusses ‘‘right‑sizing’’ and rebalancing
Get AI-powered insights, summaries, and transcripts
Subscribe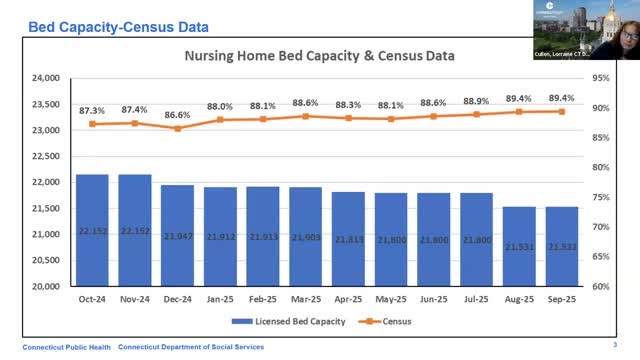
Summary
State health and social services staff told a public meeting the quarter ended Sept. 30, 2025, averaged 89.2% nursing‑home occupancy while officials and stakeholders said Connecticut has made substantial progress shifting long‑term care toward home‑and‑community based services but regional gaps and housing shortages remain.
At a Department of Public Health meeting on Oct. 9, 2025, state staff reported that average nursing‑home occupancy for the quarter ended Sept. 30, 2025, was 89.2%, up from 88.3% the previous quarter and reflecting a substantial decline from pandemic-era vacancy levels.
The statistic matters because Connecticut officials and long‑term care stakeholders said during the meeting that the state has made measurable progress toward ‘‘right‑sizing’’ its nursing‑home capacity while expanding home‑and‑community‑based services (HCBS). Still, participants said regional workforce shortages, housing constraints and local access needs mean the system remains a work in progress.
Nick Mazzotto, representing the Department of Social Services, presented the quarterly census figures and told the panel the quarter ended Sept. 30, 2025, had an average occupancy of 89.2%. Lorraine Cullen, branch chief for healthcare quality and safety at the Department of Public Health, said Connecticut currently has 192 nursing homes.
Stakeholders and legislators on the call cited a shift since the COVID‑19 public health emergency. Mazzotto said there are about 2,328 unoccupied beds statewide now, compared with 6,097 unoccupied beds reported for the quarter ended June 30, 2021. Several participants credited providers’ adjustments and policy work for much of that change.
Matthew Barrett, a committee member, said the state has seen “remarkable change” in rebalancing long‑term care and noted the Long Term Care Planning Committee has recently considered whether the longstanding 75/25 rebalancing goal (favoring community services) should be revised. Melissa Morton said the committee’s rebalancing report—filed annually to the legislature on Jan. 1—shows Connecticut was at roughly a 70/30 split (community vs. institutional) and that in 2024 Medicaid spending for HCBS exceeded institutional spending (about 59% to 41%).
Panelists stressed that statewide percentages can mask regional variation. Mag Morelli and other members said some rural areas face staffing shortages that leave beds unused even where local access is needed. Mairead (committee member) and others noted housing shortages and lack of accessible, affordable housing also constrain residents’ ability to move out of institutional settings, keeping some people in nursing homes longer than they or the system would otherwise prefer.
Panelists also flagged workforce and stigma as recruitment and retention challenges. Barrett and others described recent legislative wage enhancements—first a temporary pandemic wage boost and later additional increases—as important interventions to stabilize the workforce, but speakers said staffing gaps persist in places.
Panelists asked staff to provide more localized capacity data and to bring forecasting resources. Mazzotto said a DSS report projecting long‑term care needs (out to about 2040) is available on the DSS website and that staff would follow up with additional information on regional capacity forecasts.
Participants also noted organizational and programmatic changes tied to rebalancing work: Mairead announced that the right‑size/rebalancing steering committee (also known as the Money Follows the Person steering committee) was sunset in September after meeting its original goals, and members were encouraged to join long‑term care planning subcommittees to focus on housing and other barriers.
Why this matters: occupancy and capacity influence where the state directs Medicaid and other resources and affect access for residents in rural and urban communities. Panelists said Connecticut has made measurable progress toward shifting care into the community, but local gaps in workforce and housing, and uneven regional demand, mean officials must continue monitoring and targeted investment.
Looking ahead, staff said they will provide committee members additional forecasting details and that the Long Term Care Planning Committee will continue reviewing rebalancing goals and metrics.
