Warren County reviews 2026 benefits proposals: pharmacy strategy, GLP-1 coverage debate, Samaritan Fund, eligibility and contribution changes
Get AI-powered insights, summaries, and transcripts
Subscribe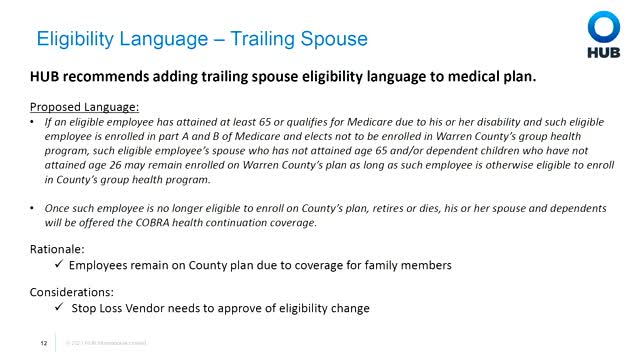
Summary
County benefits consultant Hub presented a 2026 renewal proposal including a recommended 2.5% all-in budget increase, pharmacy cost-containment results from a new PBM, debate among commissioners about coverage of GLP-1 weight-loss drugs, continued use of a Samaritan Fund for catastrophic support, a trailing-spouse eligibility recommendation, and a
Warren County benefit consultants from HUB presented the county's 2026 benefits funding and design recommendations during a work session, outlining an overall proposed 2.5% increase in the all-in benefits budget and a suite of cost-containment measures the firm recommends to preserve long-term plan stability.
Allison (benefit consultant, HUB) told commissioners the county's long‑term trend in claims has been below market and that several 2025 changes — including a new pharmacy benefit manager relationship and other utilization-management tactics — helped limit the 2026 funding need. She said HUB and county staff propose a 2.5% budget increase for 2026 that incorporates administration fees, claims, stop‑loss premiums and other benefits costs.
Pharmacy and specialty drugs took a large portion of the discussion. HUB described switching PBMs and pharmacy partners in 2025 with the goal of removing high‑cost specialty drugs from the county's net plan cost by leveraging manufacturer assistance and international sourcing. HUB estimated first‑year gross savings from the PBM change in the range discussed during prior briefings (presented last year as approximately $1.6 million to $1.9 million), and said pharmacy large‑claimants dropped out of the county's top‑10 high‑cost list for 2025.
Commissioners and staff discussed GLP‑1 class drugs (examples cited in discussion: Ozempic, Wegovy) for weight loss and diabetes management. Allison explained the county covers some of these drugs under an expanded preventive drug list but that coverage requires prior authorization and clinical criteria (for example, BMI thresholds and other diagnoses for certain drugs). Commissioners and one employee who spoke from personal experience described three policy options: (1) not covering the drugs, (2) keeping a restrictive prior‑authorization approach, or (3) making coverage less restrictive — including exploring “microdosing” or international sourcing to control costs. Several commissioners asked staff to work with HUB to develop a recommended, less‑cumbersome authorization path that preserves physician decision‑making while protecting plan costs.
HUB and county staff described the Samaritan Fund pilot introduced in 2025, which uses donor-funded assistance to cover catastrophic remaining out‑of‑pocket expenses for eligible members; staff reported positive member testimonials and that current enrollees who remain benefit‑eligible will be transitioned into the program for 2026.
HUB recommended adopting a trailing‑spouse eligibility policy that would allow spouses of employees who become Medicare‑eligible to remain on the group plan until they turn 65 (and dependents until age 26). Staff noted the change requires stop‑loss carrier acceptance; the county has 72 Medicare‑eligible plan members (38 employees, 34 spouses) and staff said they will seek stop‑loss vendor concurrence during renewal negotiations.
On plan design and contributions, HUB presented two contribution‑sharing scenarios that would modestly increase employee premium share on buy‑up options (examples shown included a 15% share on the buy‑up plan while keeping the base plan at 0% employee premium). Tammy (county benefits staff) and HUB noted the county's employer share is low compared with market benchmarks and that adjustments would shift some costs to employees to rebalance funding; presentations showed sample per‑month increases of roughly $15 for single coverage and $46 for family coverage under one 15% scenario, producing about $133,650 in additional employee contributions in the illustration.
HUB also recommended evaluating pretax benefits administration (FSAs, HRAs, HSAs) through a third‑party administrator to improve member experience; staff presented a proposal from a national vendor with a small per‑participant monthly fee. Finally, HUB recommended moving the county dental program to Delta Dental based on broader network coverage and potential discounts; staff projected a modest 1% dental cost increase before discounting and noted Delta's larger network could yield net savings.
On next steps, commissioners asked HUB and county staff to return with refined proposals, stop‑loss carrier input on trailing‑spouse language, and options to streamline prior‑authorization for GLP‑1 drugs. No binding votes on plan design or premium changes occurred at the work session; commissioners set follow‑up meetings to finalize decisions and implementation details.
