Kansas inspector general audit flags MCO prior authorization delays, inconsistent post‑acute decisions and PBM dispensing fee flows
Get AI-powered insights, summaries, and transcripts
Subscribe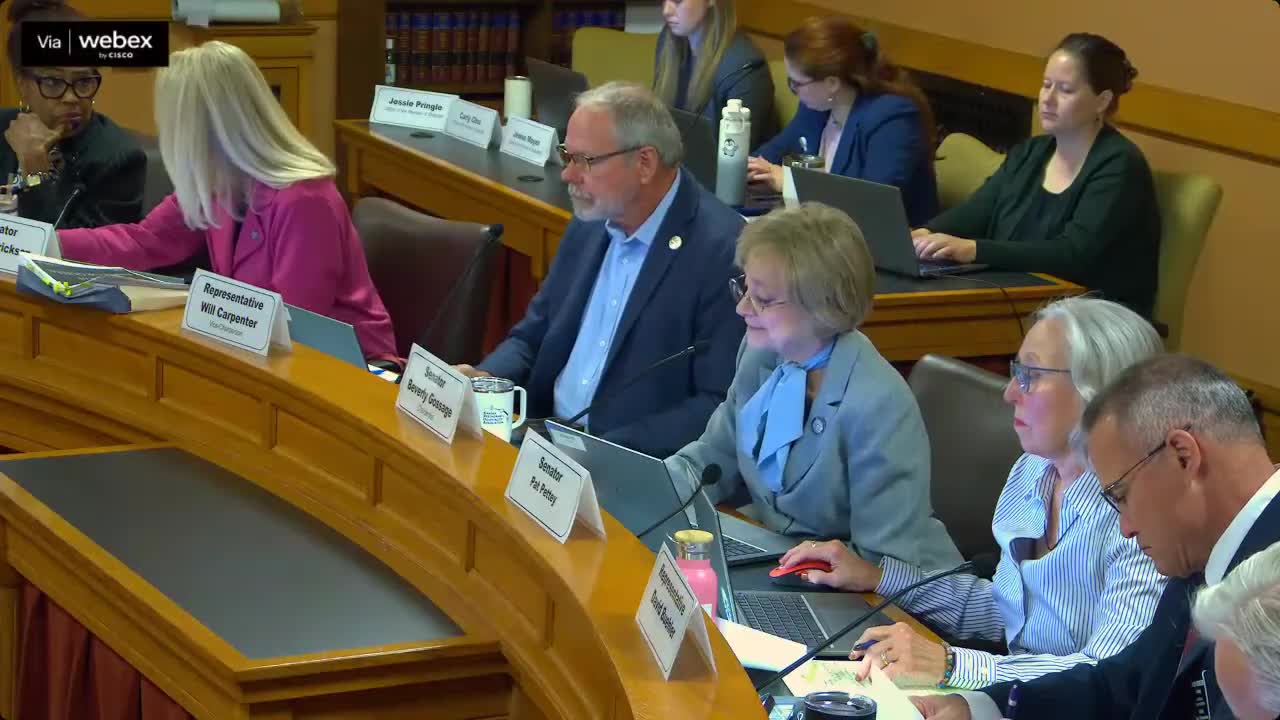
Summary
Kansas Medicaid Inspector General Steve Anderson told the Bethel committee that recent audits found prior‑authorization delays, inconsistent inpatient/post‑acute level‑of‑care determinations by managed care organizations, and concerning PBM handling of pharmacy dispensing fees.
Kansas Medicaid Inspector General Steve Anderson told the Bethel committee the office’s audits and investigations identified operational problems across managed care organizations and pharmacy benefit managers that affect providers and beneficiaries.
Anderson said a recently published prior‑authorization audit (covering Jan. 1, 2021–Dec. 31, 2023) found significant delays in peer‑to‑peer reviews that sometimes take up to seven business days and, he said, can “result[] in delays to critical care.” High denial rates force hospitals to perform additional peer‑to‑peer reviews and hire staff to manage denials.
The audit also identified a pattern of managed‑care organizations defaulting beneficiaries to observation status rather than inpatient classification. Anderson told the committee that MCOs are using commercial clinical criteria (InterQual/MCG) and that hospitals reported denials despite patients meeting clinical standards for inpatient care. He said that inconsistent post‑acute care determinations, denials of long‑term acute care, and denials of readmissions within 30 days were frequently cited by hospitals as creating avoidable readmissions and extended hospital stays.
The audit raised conflict‑of‑interest concerns where an MCO owns or controls a clinical screening tool and argued that control over algorithm design could create incentives to contain costs rather than prioritize care. Anderson also noted that third‑party claim review and coding services used by hospitals may be tied to UnitedHealth Group affiliates, creating complex ownership relationships.
On home‑and‑community‑based services the OIG is conducting a follow‑up to its 2022 HCBS review to check whether beneficiaries consistently receive at least one service per month, whether functional assessments are performed timely, and whether wait list management prioritization is equitable.
Pharmacy dispensing fees: Anderson said auditors found a $10.50 dispensing fee applied to prescriptions for many over‑the‑counter medications that are prescribed on a script, and preliminary review indicates pharmacy benefit managers (PBMs) capture a portion of those fees rather than remitting them to dispensing pharmacies. “It seems that most of it does not make it to the pharmacy, but rather gets scraped off by the PBMs,” Anderson said; auditors are still tracing funds and contractual flows.
Investigations: Anderson said the OIG screened 1,454 complaints last year and over 1,200 year‑to‑date; the office had several state‑level investigations and two federal cases accepted for prosecution, with current losses alleged near $500,000 in the cases accepted for prosecution.
Ending: Anderson said the OIG continues audits on KDHE‑MCO interactions, data‑sharing between KDHE and DCF, and a pregnant‑woman eligibility review. He said the audits and investigations produce findings that “still matter” even when direct cost savings are not identified because they substantively change operational practices.
Provenance: Inspector general testimony before the Bethel committee; audit published Oct. 2, 2025 referenced during the hearing.
