Health care access agency pauses taxonomy expansion for behavioral-health–in–primary-care measure, will use HPD analysis to refine approach
Get AI-powered insights, summaries, and transcripts
Subscribe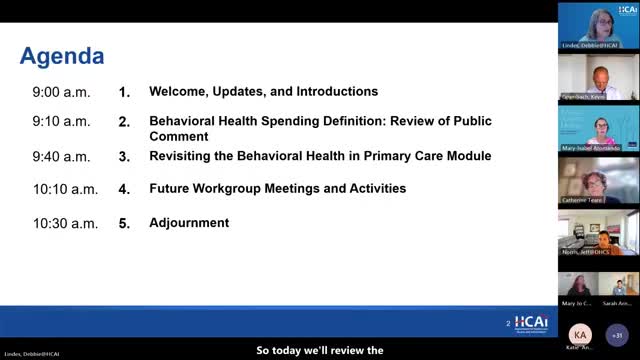
Summary
The Department of Health Care Access and Information updated its approach to measuring behavioral health spending, deciding not to expand primary-care provider taxonomies now and instead to rely on Healthcare Payments Data Program analyses and continued work with the Department of Health Care Services to incorporate Medi‑Cal data.
The Department of Health Care Access and Information (HCAI) told its investment and payment work group on a recent meeting that it will not expand the list of primary‑care provider taxonomies now for the behavioral‑health‑in‑primary‑care module, and will instead use analyses of Healthcare Payments Data Program (HPD) data over the coming year to refine the measure.
HCAI health care delivery system group manager Debbie Lindes opened the meeting and summarized public comments on HCAI’s proposed definition and methodology for measuring behavioral health spending, saying the agency received seven comment letters, including a joint letter from five organizations that represent consumers and specific populations.
The decision matters because HCAI’s methodology will be used to count behavioral‑health claims for reporting and to inform future policy tools, including an investment benchmark that the agency has delayed until at least summer 2026. HCAI staff emphasized the tension between capturing integrated behavioral‑health services delivered inside primary care and avoiding overcounting when claims data are imperfect.
Consultant Bob Seifert of the Friedman Health Care team summarized the agency’s revised plan for the behavioral‑health‑in‑primary‑care module: in the short term, HCAI will include claims that meet existing definitions for behavioral health and that fall in the outpatient professional primary‑care subcategory and will include non‑claims payments classified as primary care and behavioral‑health integration (framework category A2). "Once it is identified as a behavioral health claim . . . then the claim is examined for a primary care provider taxonomy and place of service and a service code that is in the outpatient professional primary care subcategory," Seifert said.
Seifert and HCAI staff said they will not expand the primary‑care taxonomy list now because doing so risks counting psychotherapy and other behavioral‑health services delivered outside integrated primary‑care settings. He noted the agency’s commitment that the module be "mutually exclusive, collectively exhaustive," meaning spending counted in the module must independently meet both the primary‑care and behavioral‑health definitions.
Jeff Norris, speaking for the Department of Health Care Services (DHCS), told the group that DHCS and HCAI have been discussing ways to include Medi‑Cal spending — including county behavioral‑health plan payments — in the measurement and that those discussions are ongoing. "That is definitely something we are looking into and have been talking to OCA about, for many months now," Norris said.
Work group members raised practical concerns. Several asked whether the change will affect the current 2025 data collection; HCAI clarified the 2025 collection uses last year’s taxonomy list and is unaffected. Members also pressed HCAI to use HPD to test expanded approaches that might capture collaborative care and other integrated models without systematically including nonintegrated services. Seifert said HPD analyses could help identify CPT codes and billing patterns — such as collaborative‑care codes and FQHC (federally qualified health center) billing — that indicate integrated delivery.
HCAI also addressed other public comments summarized by Lindes: a majority of commenters supported using the primary diagnosis as the principal means to flag behavioral‑health claims, though some asked HCAI to consider secondary diagnoses or additional service codes; commenters urged inclusion of G codes for dementia and of mobile clinic and crisis services as subcategories. HCAI said it will continue to evaluate G‑code use, will monitor HPD for mobile‑clinic spending (which appears minimal in HPD), and is actively working with DHCS to develop protocols to collect Medi‑Cal managed‑care and county plan spending data.
HCAI noted in the meeting that, in an earlier HPD analysis shared with the group, the outpatient professional primary‑care subcategory represented less than 2% of all behavioral‑health spending, underscoring that initial module counts may be small. The agency said portions of capitation payments will not be allocated to the module at this stage to limit reporting burdens on submitters.
HCAI also said it will move the work group from monthly to quarterly meetings beginning in mid‑December, broaden the work group’s portfolio to include primary care and alternative payment models, and expand membership to include previously participating experts in those areas. The agency plans to publish a draft 2026 data submission guide next spring that will reflect the finalized behavioral‑health spending definition and any future taxonomy updates.
What was not decided: HCAI did not adopt an expanded taxonomy or a final benchmark. The agency set a process direction: continue HPD analyses, work with DHCS on Medi‑Cal inclusion, and revisit taxonomy expansion only after analytic testing. No formal vote or board action was recorded at the work‑group meeting.
The meeting included multiple rounds of discussion and technical questions from work‑group members about county variation, the mechanics of capturing collaborative‑care billing, and the potential for double counting; HCAI acknowledged those concerns and will return to the group with analyses and updates.
Looking ahead, HCAI said it will finalize the behavioral‑health measurement definition for the data submission guide in October, share it with the board in November, and publish it in the 2026 data submission guide in spring 2026. The agency reiterated that development of an investment benchmark will continue and that the delay to summer 2026 will be used to fill data gaps identified by stakeholders.
