DHCS explains medical necessity, ORP requirement and how CYBHI interacts with IEP/LEA‑BOP billing
Get AI-powered insights, summaries, and transcripts
Subscribe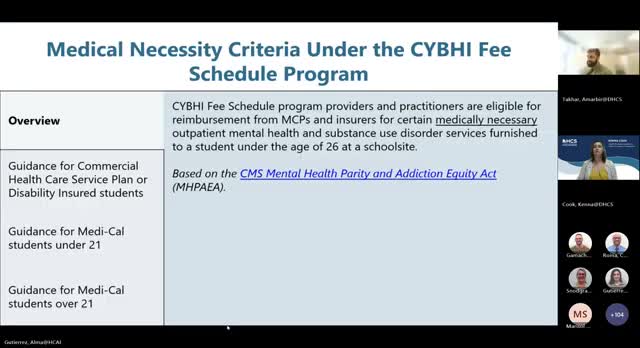
Summary
DHCS presenters described legal standards for medical necessity, when services are reimbursable for youth, the role of an ORP (ordering/referring/prescribing) clinician on Medi‑Cal claims, and guidance on billing students who are covered by IEPs or other programs.
DHCS presenters clarified how medical necessity and ORP (ordering, referring, prescribing) requirements affect reimbursement under the CYBHI fee schedule and explained how the fee schedule interacts with other school reimbursement streams.
Medical necessity standards: Amar Takkar said CYBHI services must meet medical necessity criteria to be reimbursed by Medi‑Cal managed care plans and commercial insurers. He noted statutory definitions in California law, citing the Mental Health Parity framework and referencing California Health and Safety Code and Insurance Code provisions discussed in the webinar. Takkar described medically necessary services as those that “prevent a condition from worsening, prevent the development of additional health problems, or maintain or improve a child's current health status,” and said determinations must be made case by case.
ORP and claims requirements: DHCS staff explained that an ORP must be a licensed practitioner authorized under state law to order, refer or prescribe services for Medi‑Cal beneficiaries and that for Medi‑Cal claims the ORP name and NPI must appear on the claim when the rendering provider is an unlicensed practitioner (such as a CWC). Takkar said an ORP “cannot bill Medi‑Cal independently for those services” but is required on claims for Medi‑Cal covered students to ensure services are properly authorized. DHCS staff also noted there is no limit on how many referrals an ORP can make and ORP providers do not need to supervise the rendering provider.
Interaction with IEPs and LEA‑BOP: Presenters advised providers that the same service should not be billed to two programs for the same encounter. They said general‑education students who receive behavioral‑health services outside an IEP should be billed to the CYBHI fee schedule if the LEA participates in both programs, while LEA‑BOP remains the program for IEP/IFSP‑pursuant mental health services. Presenters said DHCS will follow up in writing on some nuanced questions (for example, 504 plan cases and parent‑only encounters when the student is absent).
Claim windows and denials: During Q&A, presenters said claims must be submitted within 180 days of the date of service; claims older than 180 days would be denied unless a good‑cause exemption applied and was approved.
Ending: DHCS recommended providers document clinical findings and medical‑necessity determinations in the student record and include the ORP NPI on Medi‑Cal claims for services rendered by unlicensed practitioners to ensure claims meet program requirements.
