California outlines CYBHI fee schedule to reimburse school‑based behavioral health services
Get AI-powered insights, summaries, and transcripts
Subscribe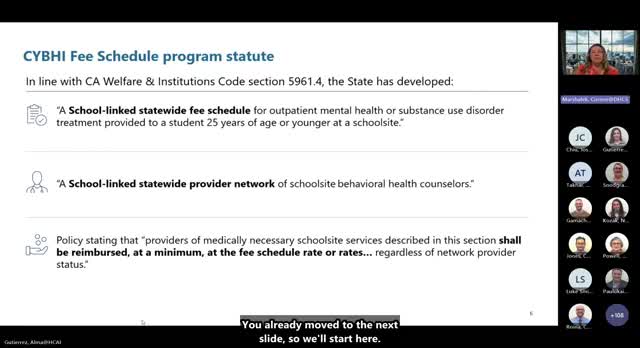
Summary
DHCS and HCAI presenters described the Children and Youth Behavioral Health Initiative (CYBHI) fee schedule statute, program goals, which insurers must pay, excluded plans, and requirements for collecting student health insurance data.
California's Children and Youth Behavioral Health Initiative (CYBHI) fee schedule requires insurers and Medi‑Cal managed care plans to reimburse medically necessary school‑site outpatient behavioral health and substance‑use services for students under age 26, program officials said Thursday. Corine Marshallek of the California Department of Health Care Services (DHCS) opened the webinar by citing the statutory basis: “the CYBHI fee schedule program statute, California welfare and institutions code section 5,961.4,” and said the law creates statewide fee rates and a school‑linked provider network to increase access.
The fee schedule is designed to establish a predictable, state‑set reimbursement model for school‑site services and to expand which practitioners are eligible for payment, Marshallek said. DHCS officials said the program aims to reduce contracting and rate‑negotiation burdens for local education agencies (LEAs) and institutions of higher education (IHEs) by using a third‑party administrator to handle claims and remittances.
Why it matters: LEAs and IHEs that participate can obtain reimbursement from Medi‑Cal managed care plans, Medi‑Cal fee‑for‑service, commercial health plans and disability insurers for eligible students, potentially offsetting school behavioral‑health costs. Marshallek said participating LEAs must collect student insurance information for reimbursable encounters so claims can be submitted.
What insurers and plans are covered and excluded: DHCS staff listed four insurer types required to reimburse under the CYBHI fee schedule (Medi‑Cal managed care plans, Medi‑Cal fee‑for‑service, health care service plans and disability insurers) and named several exclusions shown in the webinar: federal plans, self‑funded employer plans, high‑deductible plans that have not met deductible, school education plans tied to IEPs/504 plans, and Medi‑Cal share‑of‑cost plans where the deductible has not been met. Marshallek said that providers must still supply medically necessary services to students who lack covered insurance but may use alternate funding sources.
Insurance data collection requirements: Marshallek explained that LEAs and IHEs and participating designated providers must collect minimum necessary student insurance data to bill: student first and last name, date of birth, insurer name, subscriber name, member ID and group number, and that the insurance data must be current “each time the service is billed under the CYBHI fee schedule program.” The presenters added that LEAs are not required to collect insurance data for every enrolled student — only for students for whom they will seek reimbursement.
What officials said about implementation support: DHCS and HCAI presenters said LEAs must show systems for collecting insurance data as part of cohort participation. Marshallek and other presenters noted DHCS is working with a third‑party administrator and exploring ways to facilitate access to commercial insurance data but that no statewide portal currently exists.
Ending: DHCS said the fee schedule is intended to expand access and streamline reimbursement; LEAs and IHEs should review cohort requirements and prepare systems for targeted insurance data collection if they plan to bill under CYBHI.
