County providers warn of increased uninsured caseloads as Medicaid rules change in 2027
Get AI-powered insights, summaries, and transcripts
Subscribe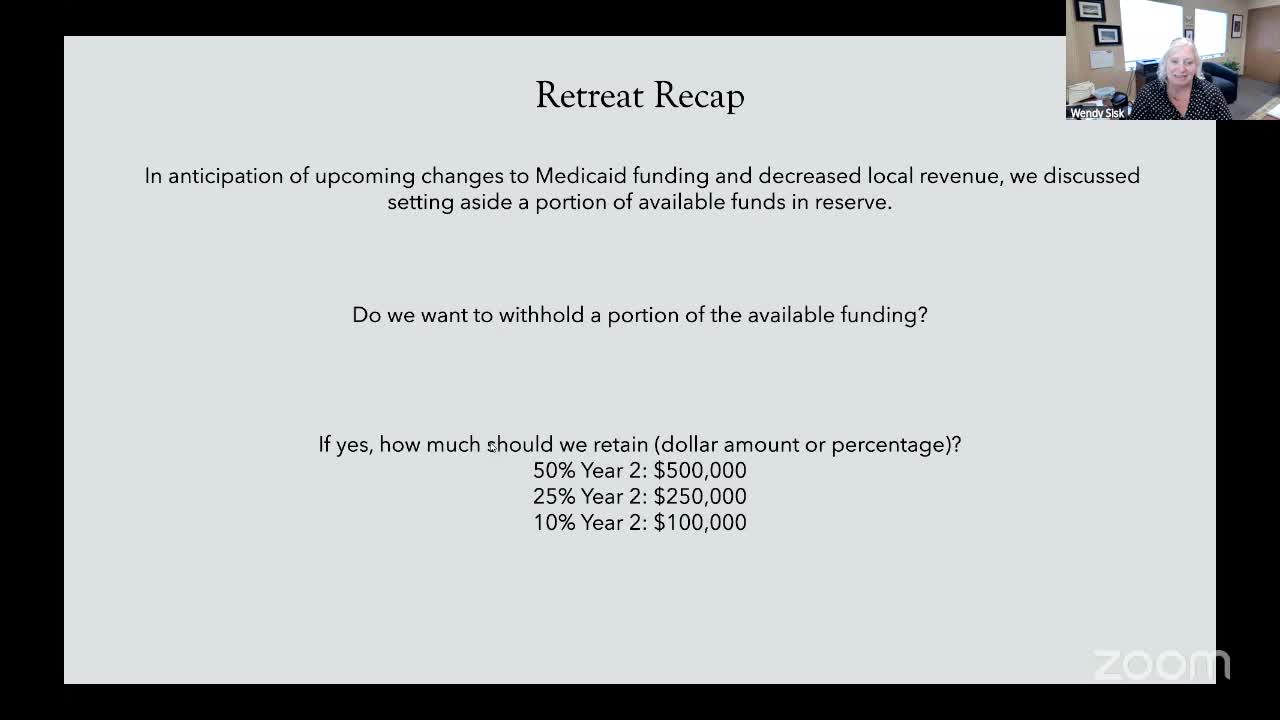
Summary
Behavioral-health providers told the Clallam County advisory board that changes to Medicaid — including work/reporting requirements and a shorter retroactive coverage window — will likely increase the county’s uninsured population beginning Jan. 2027 and put pressure on local safety‑net providers.
Behavioral‑health providers and county staff told the Clallam County Behavioral Health Advisory Board on Sept. 9 they expect a rise in uninsured clients beginning in January 2027 as federal and state changes to Medicaid enrollment and verification take effect.
“What we know at this point is that the legislature approved a 1% cut across Medicaid…starting in 2027, we anticipate additional people becoming unenrolled in Medicaid because of additional reporting requirements and work requirements,” Wendy Sisk said during a presentation on the likely impacts. “The other change that's happening is that retroactive [coverage] is changing from 90 days to 30 days.”
Providers said the administrative burden of re‑enrollment and verification could leave working—but non‑disabled—Medicaid recipients temporarily without coverage, creating an increase in unfunded visits and services. One provider described how even modest contract rates currently paid through local behavioral‑health funds are below standard Medicaid reimbursement and are already difficult to operate under; if more clients lose coverage, demand for county-funded “unfunded/underfunded” services could rise.
County staff described mitigation options under discussion, including holding a contingency from the 2026–27 RFP to redeploy in 2027, monitoring utilization, and using reserves if needed. Staff and providers emphasized the need for timely reporting and data collection to target funds where they will be most effective rather than adopting a one‑size‑fits‑all approach.
No regulatory change was made by the board; the discussion informed the board’s decision to withhold funds and to convene a review committee in early 2027 if evidence of increased uninsured caseloads emerges.
