Clallam County panel approves $1.8M RFP, withholds $100,000 per year to address 2027 Medicaid uncertainties
Get AI-powered insights, summaries, and transcripts
Subscribe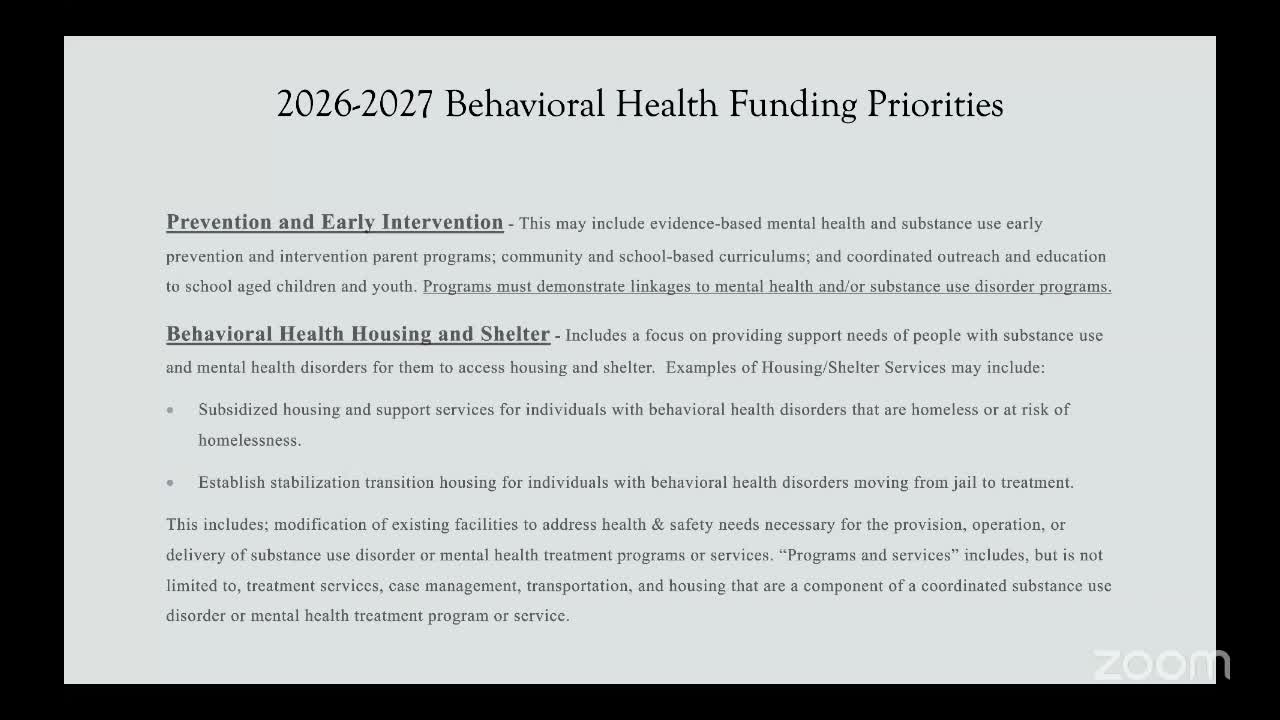
Summary
The Clallam County Behavioral Health Advisory Board approved a two-year $1.8 million request-for-proposals cycle on Sept. 9, directing staff to withhold $100,000 from each year to create flexibility for expected Medicaid coverage changes in 2027.
The Clallam County Behavioral Health Advisory Board approved a two-year $1.8 million request-for-proposals cycle on Sept. 9 and directed staff to withhold $100,000 from each year to allow the board to respond to anticipated Medicaid coverage changes in 2027.
Board members said the holdback is intended to give the board flexibility to reallocate funds in early 2027 after the effects of federal and state Medicaid changes — including new work or reporting requirements — become clearer. “We would deploy a million in total in the first year, and then a portion of that,” a county staff member said when describing how the withheld funds would be managed.
The decision followed extended discussion about whether to run a two-year funding cycle or a one-year cycle given rising uncertainty about Medicaid enrollment and reimbursement. Public-health and provider representatives described likely increases in uninsured clients after January 2027 and urged caution in committing the full two-year amount now.
Wendy Sisk, a behavioral-health provider representative, summarized the expected change: “What we know at this point is that the legislature approved a 1% cut across Medicaid…starting in 2027, we anticipate additional people becoming unenrolled in Medicaid because of additional reporting requirements and work requirements.” She told the board that the retroactive reimbursement period also is being shortened from 90 days to 30 days, which could reduce reimbursements for providers who discover coverage gaps after services are delivered.
Board members ultimately voted to structure the RFP as a two-year cycle with $1,800,000 available (split evenly as $900,000 per year) and retain $100,000 from each year — a $200,000 reserve — to be redistributed in 2027 to programs serving unfunded or underfunded clients if evidence shows a need. The motion passed on a voice vote; members voiced “aye” and no opposing votes were recorded. The motion text as read at the meeting said the withheld funds would be “redistributed to unfunded or underfunded programs” in 2027.
Officials described a practical process for the reserve: award contracts for the full two‑year requested amounts during the RFP process but hold back the agreed reserve and reconvene a review committee in early 2027 to collect up‑to‑date utilization and shortfall information from funded agencies. That committee would recommend how to allocate the held funds based on need and available data. The board discussed the risk that agencies might budget differently knowing a mid‑stream reallocation could occur, but members agreed the holdback provides a measured approach to an uncertain funding environment.
The RFP timeline shared at the meeting calls for the county to post the RFP on Sept. 16, close applications Oct. 20 at 3 p.m., conduct interviews Nov. 3–7, and make funding recommendations to the advisory board in a special meeting on Nov. 14; contracts would then be executed to begin Jan. 1. County staff said they will ask applicants to submit full two‑year budgets so the review committee has visibility into program needs even if the second‑year pool starts smaller.
Board members emphasized that the reserve aims to protect frontline, safety‑net services that may face higher demand if Medicaid disenrollment rises. “We are trying to be responsible in how it’s being allocated and spent over this time frame,” one member said as the board closed the vote.
