OCA to monitor mobile clinics and county behavioral health spending; public comment and benchmark timeline outlined
Get AI-powered insights, summaries, and transcripts
Subscribe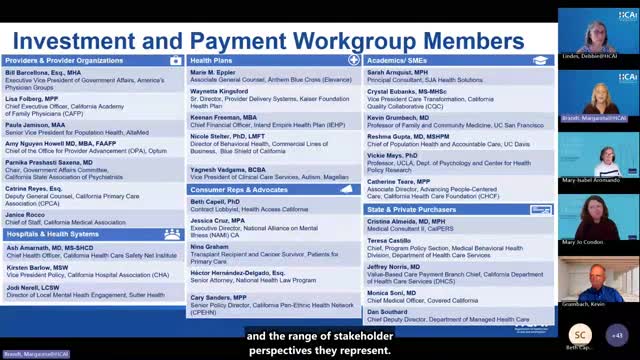
Summary
OCA staff told the Investment and Payment Work Group they will continue to monitor mobile clinic and crisis‑care delivery via HPD, work with DHCS to capture county behavioral health spending, and delay a final investment benchmark until supplemental analyses are completed.
Office of Healthcare Affordability staff told the Investment and Payment Work Group they received several key requests from the OCA board when presenting the behavioral health measurement proposal: continue monitoring mobile clinic and crisis-care delivery via HPD, develop a process to capture county behavioral health plan spending, and pursue alternative approaches to identify out‑of‑pocket/out‑of‑plan consumer spending.
Margaret Brandt, assistant deputy director for health system performance at OCA, said the board supported removing mobile clinic services and long‑term care from the proposed reporting subcategories because HPD shows negligible spending in those subcategories. Brandt added the board nevertheless urged OCA to use HPD going forward to monitor mobile clinic services and crisis care as delivery patterns change. “We will be collecting data on mobile clinic services spending and long term care spending for behavioral health,” Brandt said; OCA’s proposal would not present those as separate subcategories but would retain them in overall reporting.
Board members also stressed the importance of capturing spending by county behavioral health plans for medical‑specialty behavioral health services. Brandt said OCA is meeting regularly with the Department of Health Care Services (DHCS) to explore how to measure county behavioral health spending and hopes to report back to the work group this winter. Separately, OCA noted it plans to propose that Medi‑Cal managed care plans submit behavioral health spending data next fall, using a similar framework to commercial and Medicare Advantage plan submissions.
The board asked for a better approach to measuring out‑of‑pocket and out‑of‑plan consumer spending on behavioral health services. OCA reported that prior analysis using the Medical Expenditure Panel Survey produced limited actionable results and that staff are developing an alternate analytic plan and timeline to address that gap.
On timing, OCA recommended postponing adoption of a behavioral health investment benchmark until at least next summer while staff complete supplemental HPD analyses to refine the measurement methodology and to produce inputs for a benchmark recommendation. OCA also outlined next steps in the public process: the public comment period on the proposed definition closes September 3; OCA will review public comments at the September work group and advisory committee meetings and aims to finalize the definition in October for use in its 2026 data submission guide. OCA added it will expand the work group’s scope, move to quarterly meetings after September, and invite additional members to support broader work on behavioral health, primary care, and alternative payment models.
There were no formal board votes reported at the meeting; the matters discussed were procedural and analytic. Work group participants asked OCA to return with updates on county and Medi‑Cal data availability and on any alternative approaches to measuring out‑of‑pocket spending.
