HPD commercial claims: mental health drives spending; substance use disorder care concentrated in facilities
Get AI-powered insights, summaries, and transcripts
Subscribe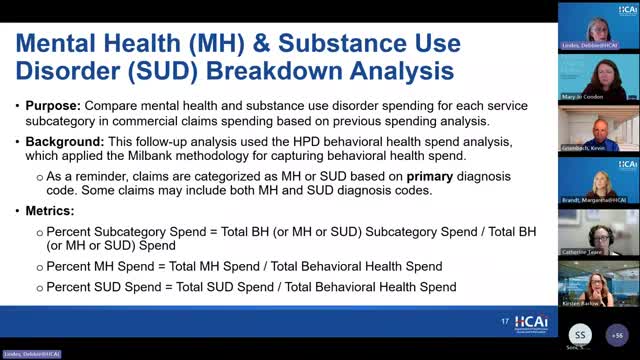
Summary
OCA presented Healthcare Payments Data Program analyses showing mental health accounted for roughly seven of eight commercial behavioral health dollars from 2018–2023; substance use disorder (SUD) spending grew faster but remained a smaller share and was concentrated in inpatient and residential facilities.
OCA staff presented new analyses from the Healthcare Payments Data Program (HPD) showing, for commercial claims, mental health services accounted for the large majority of behavioral health spending from 2018 through 2023 while spending for substance use disorder (SUD) services remained concentrated in facilities.
According to the HPD analysis discussed at the work group, total commercial behavioral health spending rose about $2.0 billion (about 65%) between 2018 and 2023. In 2023, commercial claims spending for mental health was about $4.5 billion; spending for substance use disorder services was about $623 million. Because mental health spending comprises most dollars, it largely determines which service subcategories dominate overall behavioral health spending. OCA staff noted mental health spending has shifted from inpatient and emergency settings toward outpatient and residential settings, while outpatient professional SUD services declined and most SUD dollars were in inpatient and residential facilities.
The analytic approach followed the Milbank process map for classifying behavioral health claims. A claim is categorized as behavioral health if it carries a primary behavioral health diagnosis or a screening/assessment service code; after that, place-of-service and service codes determine subcategory. OCA emphasized these HPD analyses are commercial claims only and that year-to-year results may change as HPD data quality and completeness evolve.
Work group members raised questions about interpretation and next steps. Beth asked for behavioral health spending presented as a share of overall commercial health spending to help the OCA board place the findings in the broader financial context. Kirsten suggested comparing spending trends with changes in the supply of licensed facilities and clinicians, noting access constraints could shape utilization patterns. Hector and other participants observed that the claims analysis does not show which services patients actually received (for example, whether medications for opioid use disorder were provided in residential stays) and recommended follow-up analyses to link settings with specific services and medications.
OCA staff said additional HPD analyses are planned to support measurement refinement and the development of an investment benchmark, including payer-level trends, demographic breakdowns, and decomposition into price versus utilization drivers. Staff also reminded the group that HPD commercial claims do not capture Medi‑Cal or many county behavioral health expenditures; OCA is working with the Department of Health Care Services (DHCS) and HPD to identify county and Medi‑Cal information for inclusion in future analyses.
The discussion identified three distinct follow-up needs: more contextual benchmarks (behavioral health as share of total commercial spending), supply-side measures (licensed facilities and workforce), and service-level linkage (whether settings provide specific evidence-based treatments and medications). No formal votes occurred; staff directed analytic follow-up with HPD and committed to reporting additional disaggregations and sensitivity tests.
