HPD commercial claims: mental health drives spending; SUD concentrated in facilities, OCA shows
Get AI-powered insights, summaries, and transcripts
Subscribe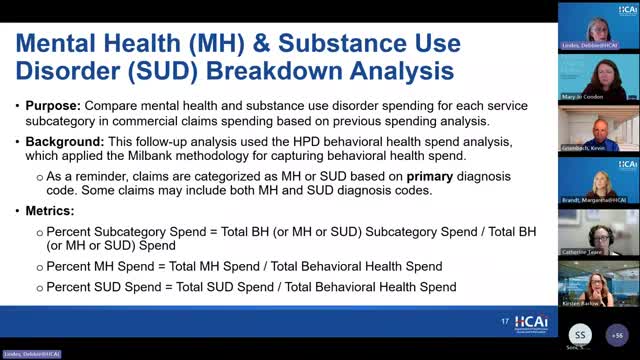
Summary
An analysis of commercial claims in the state Healthcare Payments Database (HPD) presented Aug. 20 showed mental health services accounted for roughly seven of every eight commercial dollars spent on behavioral health in 2023 while substance use disorder services represented about 12.2 percent and were concentrated in inpatient and residential facilities, OCA staff said.
HPD commercial claims: mental health drives spending; SUD concentrated in facilities, OCA shows An analysis of commercial claims in the state Healthcare Payments Database (HPD) presented Aug. 20 showed mental health services accounted for roughly seven of every eight commercial dollars spent on behavioral health in 2023 while substance use disorder services represented about 12.2 percent and were concentrated in inpatient and residential facilities, OCA staff said. OCA staff reported that total commercial behavioral‑health spending rose by about $2,000,000,000 — roughly a 65 percent increase — from 2018 to 2023. In 2023, OCA cited roughly $4,500,000,000 in commercial mental‑health claims spending and $623,000,000 in commercial SUD claims spending. Mental‑health spending grew about 63 percent over the period; SUD spending grew about 80 percent, increasing the SUD share of commercial behavioral‑health spending by about one percentage point to 12.2 percent in 2023. The analysis followed the Milbank categorization approach used to sort claims into service subcategories. OCA noted that the three largest commercial subcategories in 2023 were outpatient professional non‑primary‑care, pharmacy and inpatient facility claims, which together comprised more than 70 percent of commercial behavioral‑health spending. For mental health the top categories were outpatient professional non‑primary‑care, pharmacy and inpatient facilities; by contrast, most commercial SUD dollars were in inpatient and residential facility settings and the outpatient professional share for SUD was small and declining. Debbie Lindes cautioned that the HPD is an evolving data source and that year‑to‑year results can change as data quality and completeness improve: "please keep in mind that the use of HPD data for this type of analysis is quite new, and as the HPD continues to mature, year to year results may vary due to changes in data quality and completeness." Vinayak, who led the presented analysis, added that the outpatient professional primary‑care piece in the Milbank view is slightly narrower than OCA’s prospective definition and does not include the additional taxonomies currently under consideration for OCA’s primary‑care definition. Participants responded that the commercial‑only nature of these HPD analyses limits conclusions about overall system capacity and access. OCA staff reiterated that commercial claims do not capture Medi‑Cal or county behavioral‑health spending and that OCA is actively working with DHCS and the HPD team to understand how county and Medi‑Cal managed‑care behavioral‑health spending might be captured in future analyses. Work group members asked for follow‑up analyses, including: (1) splitting spending by payer type and demographic subgroups, (2) decomposing spending trends into price versus utilization drivers, and (3) investigating the decline in outpatient professional SUD claims to determine whether it reflects unmet need, coding shifts, or other system changes. OCA said it plans those supplemental analyses to inform a behavioral‑health investment benchmark deliberation expected next summer.
