CalPERS to move many pharmacy benefits to CVS Caremark, SilverScript to administer Medicare pharmacy
Get AI-powered insights, summaries, and transcripts
Subscribe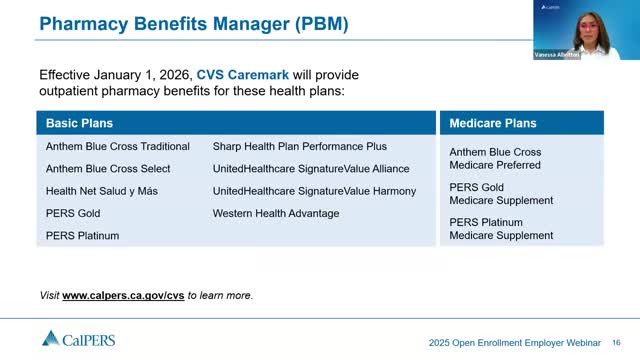
Summary
CalPERS told employers that CVS Caremark will replace OptumRx as the pharmacy benefits manager for many basic and Medicare plans effective Jan. 1, 2026, with SilverScript administering pharmacy benefits for certain Medicare supplements; the agency mailed notices to affected Medicare members and scheduled a Sept. 18 webinar.
CalPERS announced that CVS Caremark will replace OptumRx as the pharmacy benefits manager (PBM) for numerous CalPERS health plans effective Jan. 1, 2026. Rob Jarzombek, chief of the Health Plan Research and Administration Division, said the change affects outpatient pharmacy benefits for several Anthem, Health Net, Sharp, UnitedHealthcare and Western Health Advantage basic plans and some Medicare supplements.
The change matters because pharmacy formularies, copays and prior-authorizations may change for affected members. “There will be some formulary changes and there may be changes to copays,” Jarzombek said. He added plans are in place to transfer approved prior authorizations and to support members during the transition.
CalPERS said Medicare members enrolled in Anthem Medicare Preferred and some PERS Gold and PERS Platinum Medicare supplements will have pharmacy benefits administered by SilverScript, an affiliate of CVS. “SilverScript and CVS work together, and really the only difference is branding and the appearance of the materials members receive,” Jarzombek said. CalPERS mailed letters to impacted Medicare members introducing SilverScript and said it is updating FAQs online.
CalPERS encouraged employers and members to review the PBM transition resources and to join a special PBM webinar on Sept. 18. The agency also said most members can continue using their current pharmacy and that automatic transfers of mail-order prescriptions are being arranged, though members can change fulfillment channels once CVS is live.
Who is affected: Jarzombek listed Anthem traditional and selective basic plans and Anthem’s Medicare Advantage plan; Health Net Salud y Más basic and Medicare plans (PERS Gold and PERS Platinum); Sharp Health Plan basic; UnitedHealthcare Alliance and Harmony basic; and Western Health Advantage basic. CalPERS said Blue Shield HMOs and Kaiser plans are not affected.
CalPERS said both basic and Medicare formularies will be posted on CVS and CalPERS websites during open enrollment so members can review tiering and copay information. The agency advised members to watch communications from CVS and SilverScript and promised additional FAQs on calpers.ca.gov.
For more information: CalPERS is conducting a PBM webinar on Sept. 18 and has posted mailed notices and online materials for impacted members.
