Work group discusses consent, court orders and stigma for justice‑involved people needing court‑ordered SUD treatment
Get AI-powered insights, summaries, and transcripts
Subscribe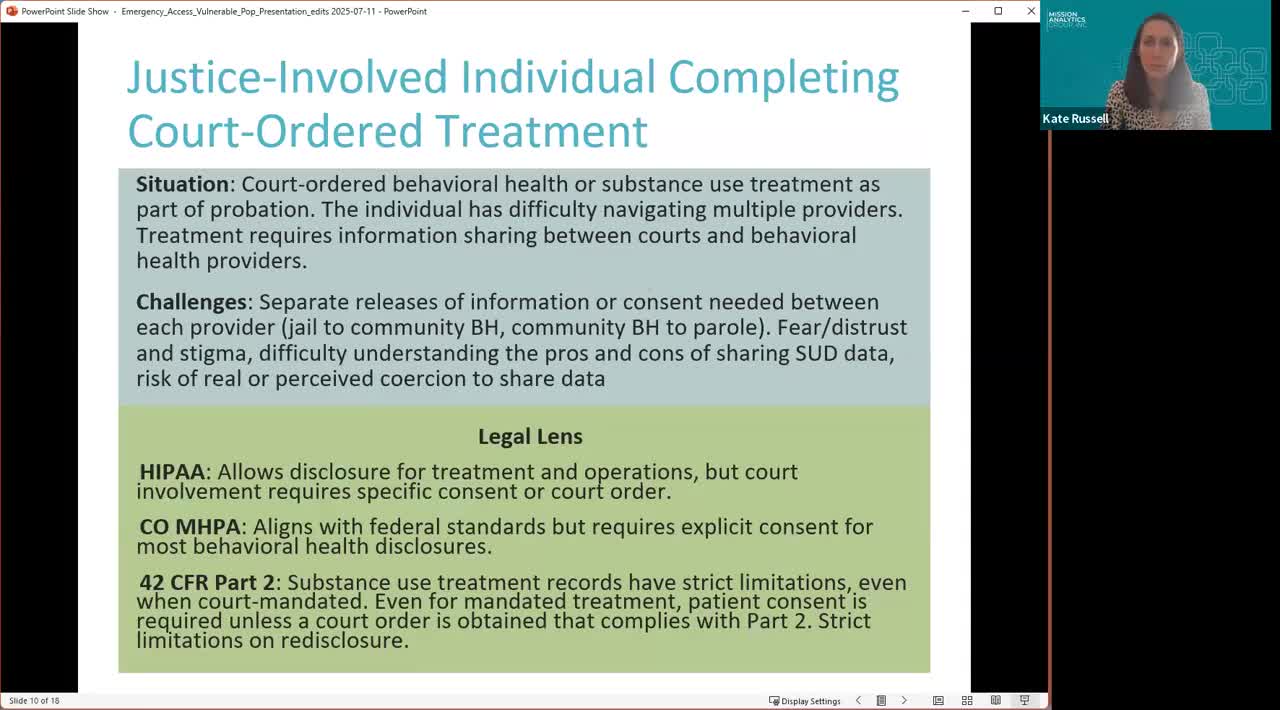
Summary
Mission Analytics outlined how court‑ordered substance‑use disorder treatment can require specific releases of information and multiple, localized data‑sharing agreements, and the legal presenters warned courts and providers must meet strict documentation and specificity requirements under HIPAA, 42 CFR Part 2 and Colorado law.
Mission Analytics told the Consent Repository Feasibility Study work group that people transitioning from the criminal justice system face fragmented data sharing and additional legal hurdles when court‑ordered treatment requires verification of care.
The consultants said that county‑level contracts, separate jail health vendors and the need for specific releases of information make it difficult for community providers and parole officers to verify treatment quickly. “In this case, the parole officer needs verification of treatment to fulfill that court ordered, requirement,” Kate Russell, an analyst with Mission Analytics, said when introducing the persona.
Why it matters: justice‑involved people commonly lack navigation support after release, creating friction in obtaining court‑required documentation and risking noncompliance. Legal consultant Matthew Moore told the group that if a disclosure is not for treatment, payment or health‑care operations, HIPAA generally requires explicit patient consent or a court order; for substance use and mental‑health records, 42 CFR Part 2 and the Colorado Mental Health Practice Act impose heightened requirements and limit blanket disclosures.
Key points from the discussion - Fragmented contracts and data agreements: Mission Analytics noted jails and justice health services are highly localized (county‑level vendor contracts), requiring separate agreements to share data with community providers and parole officers. - Consent versus court orders: Moore emphasized that courts can issue orders to compel disclosure, but orders must be narrowly tailored — specifying the exact types of PHI and purposes — and cannot authorize broad, blanket access to all mental‑health or substance‑use records. - Stigma and coercion concerns: presenters warned that justice‑involved people may distrust systems and feel coerced into consenting. Kate Russell said individuals may “feel like they absolutely have to” share sensitive information to comply with court requirements, and the group discussed time‑limited or narrowly scoped consents to reduce unnecessary disclosure. - Payment and third parties: a participant named Jane observed that court‑ordered treatment may bring payers (insurance) into the picture; Moore clarified that insurers involved for payment have HIPAA‑permitted access for payment purposes, but that does not authorize insurers to disclose patient data to the court without separate authorization.
Design considerations discussed - The repository should support fine‑grained recipient controls (patients specifying which providers or categories may receive records) and time‑limited consents to limit overbroad sharing. - Distinguishing voluntary consent from mandated disclosures and adding safeguards where justice‑related data intersects with behavioral‑health data to prevent inadvertent sharing that could prejudice care.
No formal action was taken; presenters asked the work group for design feedback on how to represent mandated disclosures versus voluntary consents and what privacy safeguards the repository should enforce.
