House committee advances bill to speed prior‑authorization decisions and create working group
Get AI-powered insights, summaries, and transcripts
Subscribe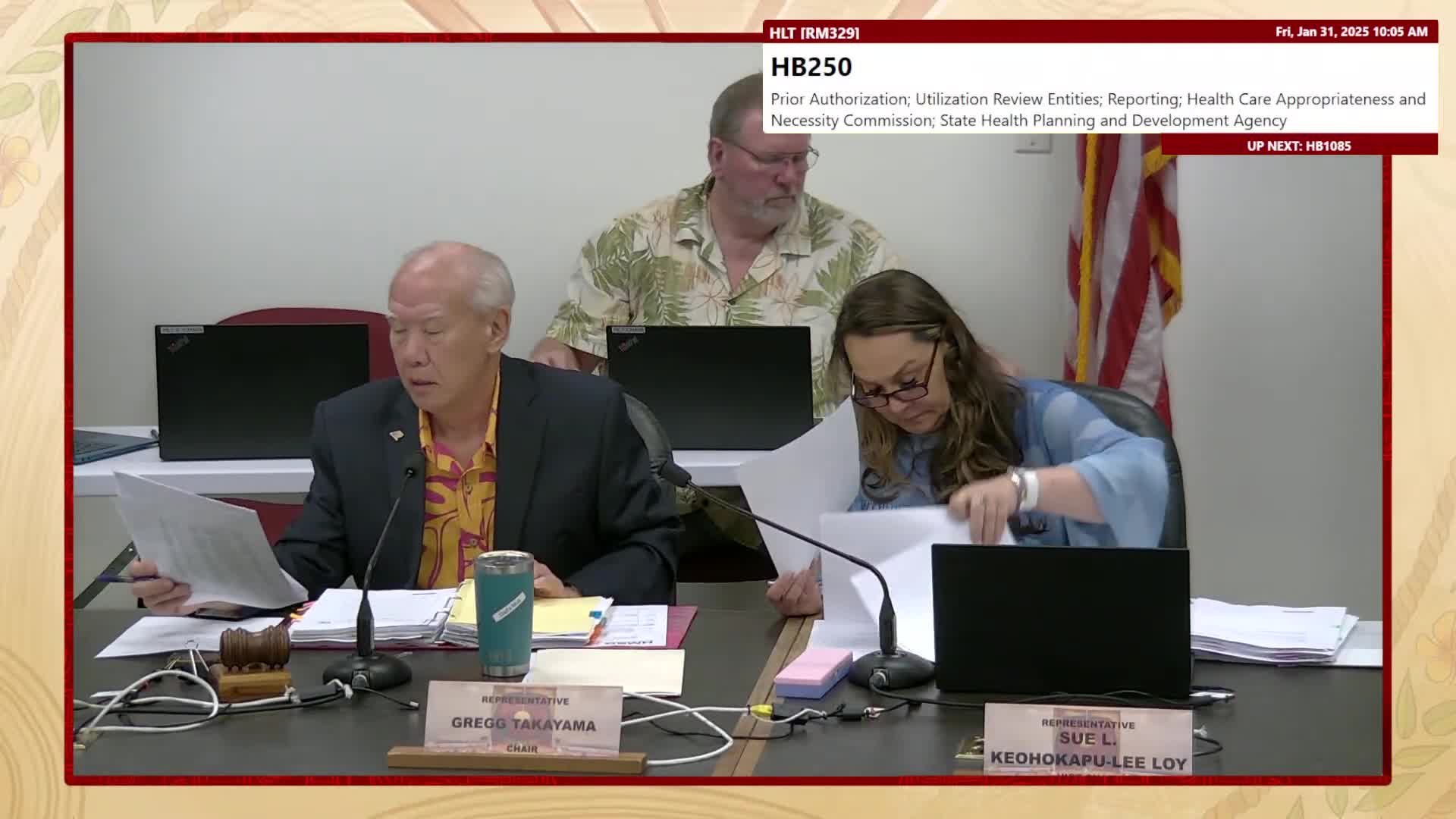
Summary
HB250, a multifaceted reform to increase transparency and shorten prior authorization turnaround times, advanced with amendments to create a working group, add lab/diagnostic services, and adopt timelines for auto‑approval if plans do not act.
Lawmakers advanced House Bill 250 after extensive testimony from clinicians, patient advocates and insurers about the burdens and delays associated with prior authorization.
Dr. Jack Lewin, administrator of the Hawaii State Health Planning and Development Agency, proposed a two‑part approach: require reporting on prior‑authorization parameters to a state body and form a working group to agree on standards that could be automated for common conditions. He urged the committee to include laboratory and diagnostic tests in the list of services subject to the process and to adopt a temporary working group rather than a permanent commission.
Insurers told the committee federal Medicare/Medicaid (CMS) rules effective in 2026–2027 would address many concerns and urged avoiding duplicative state reporting. HMSA and Kaiser proposed placing reporting authority under the insurance commissioner (DCCA) to match regulatory jurisdiction and suggested aligning with upcoming federal electronic prior authorization requirements.
The chair moved an amendment to add automatic approval timelines in limited circumstances: for non‑urgent care, a request would be deemed approved if the utilization review entity fails to act within 48 hours (with a 24‑hour extension if additional information is requested); for urgent care, the deeming period would be 24 hours (with a 12‑hour extension for requested information). The committee also added lab and diagnostic tests to the covered services list, replaced “commission” language with “working group,” and changed references from “commissioner” to “agency.” Report language will instruct future committees to refine the working group’s composition.
Committee action: members adopted the amendments and moved HB250 forward with the changes. Supporters described the amendments as an attempt to accelerate access while preserving clinical review; payers urged alignment with forthcoming federal requirements.
Why it matters: Prior authorization was cited as a recruitment and retention problem for clinicians, a patient care delay, and a productivity burden. The bill’s deeming timelines and a working‑group approach aim to produce standards that can be automated to reduce delay.
