Senators press VA nominee John Bartram on staffing, wait times and contract reviews
Get AI-powered insights, summaries, and transcripts
Subscribe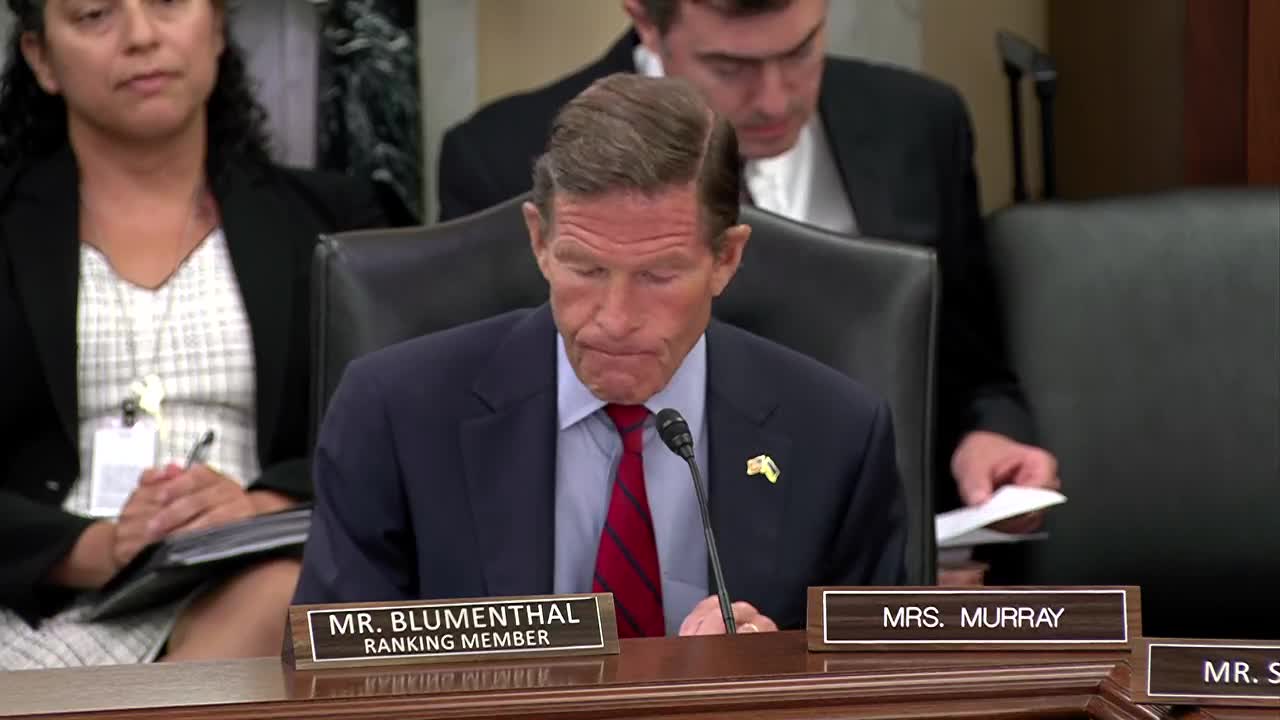
Summary
Senators questioned John Bartram about reported large staff losses, an effort to terminate or rescope thousands of VA contracts and whether those moves threaten veterans' access to care. Bartram said he supports building staffing models and that he has participated in contract review but lacks full visibility into every HR decision.
John Bartram, the nominee for Undersecretary for Health at the Department of Veterans Affairs, faced sustained questioning from senators about recent VA workforce shifts and a departmental memo describing planned contract terminations and non‑reviews.
Senator Richard Blumenthal cited news reports and told the committee that the Federal News Network had reported losses of clinicians and frontline staff, listing “1,720 registered nurses, 600 doctors, 1,150 medical support assistants, close to 200 police officers, 80 psychologists, and about 1,100 claims examiners.” Blumenthal said published investigations suggested the cuts had not reduced overall spending and asked Bartram to explain his role. Bartram said he was not involved in every HR decision and that his role as a senior adviser did not give him complete visibility into every personnel action; he said he was willing to work with the committee to develop standard staffing models and “manning documents” to determine correct staffing levels.
Senator Angus King pressed Bartram about a VA email that listed roughly 16,000 contracts the department said it would terminate or not review to avoid an estimated $13.1 billion in costs, and asked whether such a broad list could be relied upon to protect veteran care. King told Bartram he feared the department was starting with a numerical quota (first reported as 83,000 and later described as 30,000) and “working backwards.” Bartram said some contracts identified for termination were duplicative and that in other cases contracting teams were pursuing consolidation into regional or national contracts; he acknowledged he had been involved in reviewing contracts that career officials recommended for rescoping or cancellation and agreed to provide committee staff further details for the record.
Bartram also defended certain operational improvements, telling the committee the VA has expanded its electronic scheduling system and that increased scheduler throughput can improve access. But senators repeatedly emphasized that workforce planning should be built on staffing models tied to patient needs rather than top‑down quotas.
Committee members asked Bartram for data on community care wait times, the number of veterans participating in clinical trials, and a count of canceled contracts; Bartram said he would provide additional information for the record. The committee requested timely and complete documentation to assess whether the department’s staffing and contracting actions risk veterans’ access to care.
