District hears self‑funded insurance review; board seeks clearer employee education on premiums
Get AI-powered insights, summaries, and transcripts
Subscribe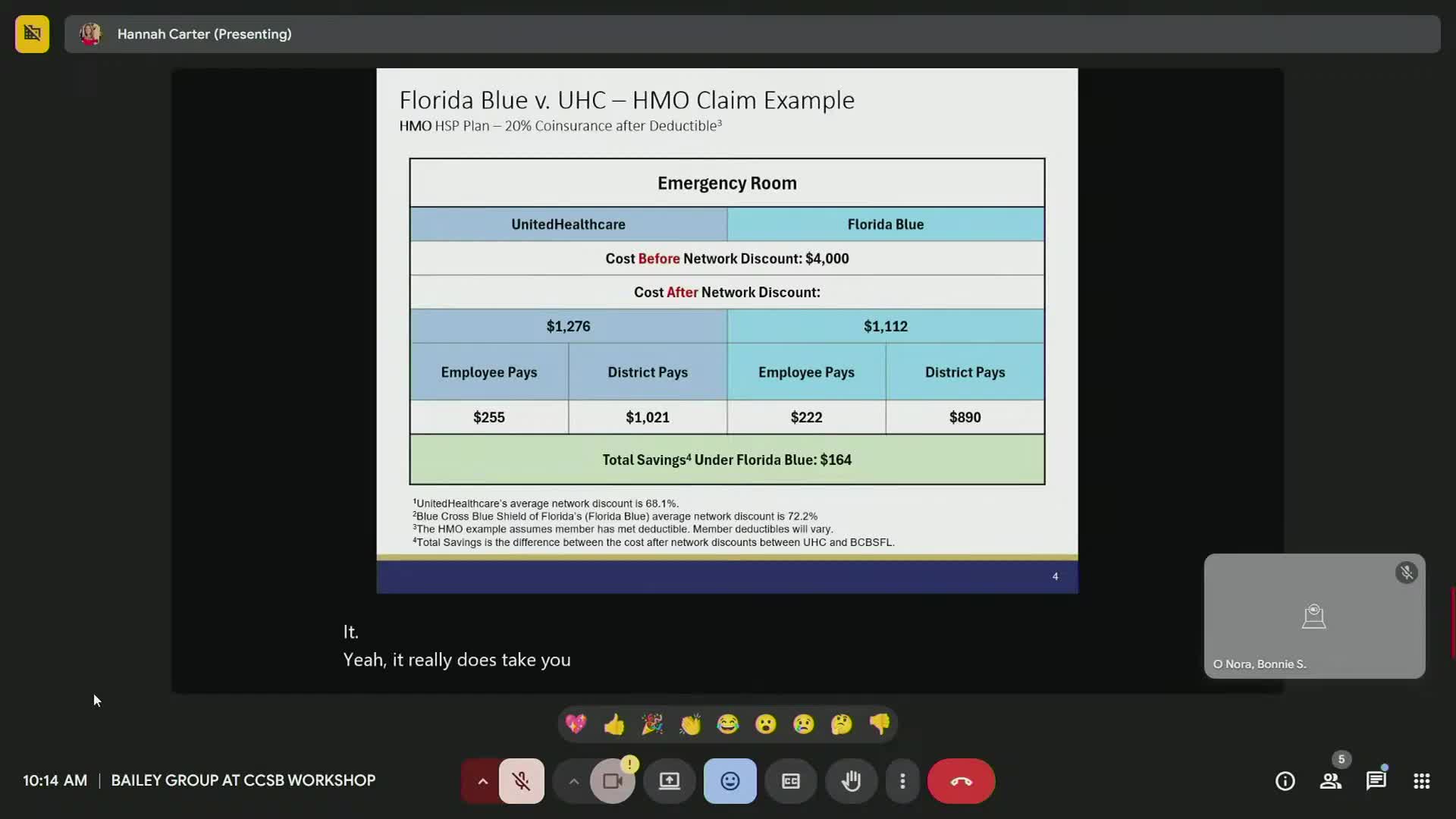
Summary
A benefits presentation at the July 29 workshop reviewed the district’s move to a self‑funded plan, projected savings and premium structure. Board members urged clearer communication and recorded virtual sessions for employees before and during enrollment.
District benefits staff and their consultant presented options and examples for the district’s self‑funded health plan at the Clay County School Board workshop on July 29, and board members called for clearer, accessible education for employees about premiums, co‑pays and how the projected savings will flow.
The consultant, identified in the meeting as Hannah, presented sample plan scenarios and said the district’s employee rates have not increased for six years. “It’s been 6 years that the rates have [been] the same for employees,” Hannah told the board when asked about historical premiums.
Why it matters: the district’s move to a self‑funded model affects monthly premiums, out‑of‑pocket co‑pays and where employees seek care (urgent care versus emergency room). Board members said employees are contacting them confused about paycheck deductions and expected out‑of‑pocket costs.
Key points from the presentation included projected plan savings and options that use either fixed co‑pays or percentage‑based cost‑sharing. The benefits presenter noted potential annual savings shown in modeling exercises but emphasized some savings are prospective (cost avoidance) rather than immediate reductions to employee paychecks. The consultant and district staff said new plan rates take effect Oct. 1, 2025, and open enrollment deadlines were already underway.
Board members and staff discussed how employees perceive the change. Several trustees said employees comparing the new plan to last year expect immediate pocketbook relief and that the presentation’s large projected savings (the consultant cited multi‑million dollar future savings in modeling) needs clearer explanation as future cost avoidance rather than instant reductions in premiums.
District staff agreed to record virtual, on‑demand benefits presentations for employees and to host vendor information sessions in multiple locations or virtually during preplanning so staff with limited travel access can view materials. The benefits consultant agreed to post recorded sessions to the district benefits site and to provide plan premium breakdowns and example monthly contributions for each plan option.
Ending: the board requested clearer, follow‑up communications targeted to employees (infographics, recorded presentations and FAQ materials) and additional vendor sessions to ensure staff understand co‑pays, deductibles and when alternative sites such as urgent care can reduce costs compared with emergency rooms.
