OCAH proposes removing mobile clinic and long‑term care subcategories from payer reporting; HPD to provide granular analysis
Get AI-powered insights, summaries, and transcripts
Subscribe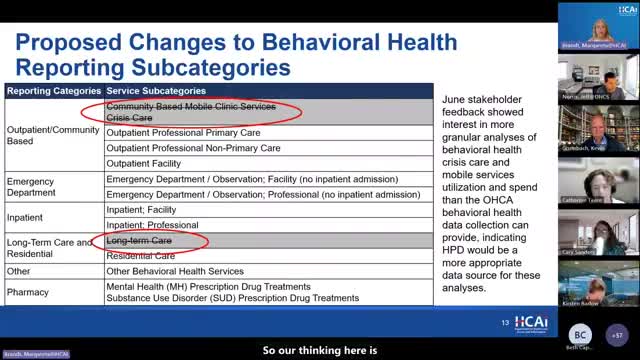
Summary
OCAH staff recommended folding mobile clinic/crisis care and long‑term care spending into broader outpatient categories for payer reporting to reduce submitter burden; HPD analyses will be used for detailed study of crisis and mobile services.
OCAH staff proposed removing the distinct reporting subcategories for mobile clinic services (and a separate “crisis care” subcategory) and for long‑term care from the payer submission template. The change would not exclude the spending from measurement, staff said; instead, those payments would be captured in broader outpatient or “other services” categories for payer reporting to reduce data submitter burden.
Staff explained that preliminary HPD analysis found commercial spending on mobile clinic services to be negligible (below one‑tenth of 1% of commercial behavioral health spending from 2018–2023) and long‑term care spending similarly small. Medi‑Cal showed modest mobile clinic spending (about 4% during 2018–2023), staff said. Because those services are both small in payer data submissions and often require more granular encounter‑level information to understand utilization, OCAH recommended using HPD for deeper analysis of crisis and mobile clinic services.
Several participants supported the change but raised caveats. Kirsten Barlow of the California Hospital Association supported removing the mobile clinic and long‑term care subcategories for the payer reporting template, noting that mobile clinic programs are largely rolled out through Medi‑Cal and county behavioral health systems that the initial payer submissions do not comprehensively capture. Beth and Carrie emphasized the importance of making clear in OCAH public materials what payer submissions include and what will be studied using HPD. Hector noted AB 988’s requirement for private plans to cover mobile crisis services and suggested OCAH monitor trends and reconsider adding the subcategories if utilization grows.
OCAH staff said the recommended change is intended to simplify reporting while preserving total spending measurement; the team committed to using HPD to monitor mobile crisis and related service utilization and to revisit subcategory definitions in future reporting cycles if warranted.
