OCAH to collect behavioral health spending data for 2024–25; benchmark deferred until more analysis
Get AI-powered insights, summaries, and transcripts
Subscribe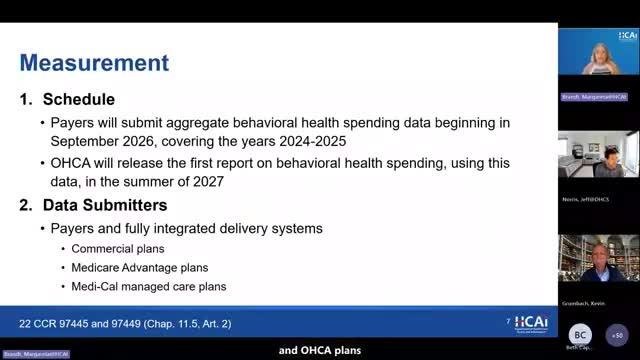
Summary
The OCAH work group said payers will submit behavioral health spending data covering 2024–25 in fall 2026, with a first OCA report expected summer 2027. The OCA board has chosen to delay adopting an investment benchmark until it has more data and HPD analyses.
OCAH Assistant Deputy Director Margaret DeBrant said payers will submit behavioral health spending data in fall 2026 covering performance years 2024 and 2025, and OCA plans to publish the first report in summer 2027. The statutory mandate, she said, requires measuring behavioral health spending relative to total health care spending and setting benchmarks intended to promote better outcomes and increased capacity.
The work group was told entities required to submit data are payers and fully integrated delivery systems that cover a minimum of 40,000 lives in the commercial, Medicare Advantage and Medi‑Cal managed care markets. DeBrant added that the detailed methodology will be published in an updated data submission guide in spring 2026 and that submitted data will be aggregated by performance year and market category.
The work group discussed the role of the Health Care Payments Database (HPD) in supplementing OCA’s reporting. DeBrant said HPD can support more granular analyses of utilization and spending — for example, to study mobile crisis services and other emerging modalities that may be sparsely represented in payer submissions. Several participants urged OCAH to be explicit in public presentations about what the payer data include and what will instead be examined via HPD analyses.
DeBrant also summarized the OCA board’s decision to postpone setting an investment benchmark. The board will revisit the benchmark next summer after additional data collection and HPD analysis; the work group’s members were told the 2026 payer submissions will be used for measurement and reporting only, not for immediate comparison to a benchmark.
The work group requested that OCAH continue to coordinate with the Department of Health Care Services (DHCS) over the summer and fall to understand how Medi‑Cal programs that do not flow through managed care (for example, some county mental health programs) might be tracked for behavioral health spending. DeBrant said the team will incorporate those follow‑up plans and clarify limits of the initial dataset in future presentations and in the data submission guide.
