DSHS outlines 1115 waiver services: caregiver supports, presumptive eligibility and social needs benefits
Get AI-powered insights, summaries, and transcripts
Subscribe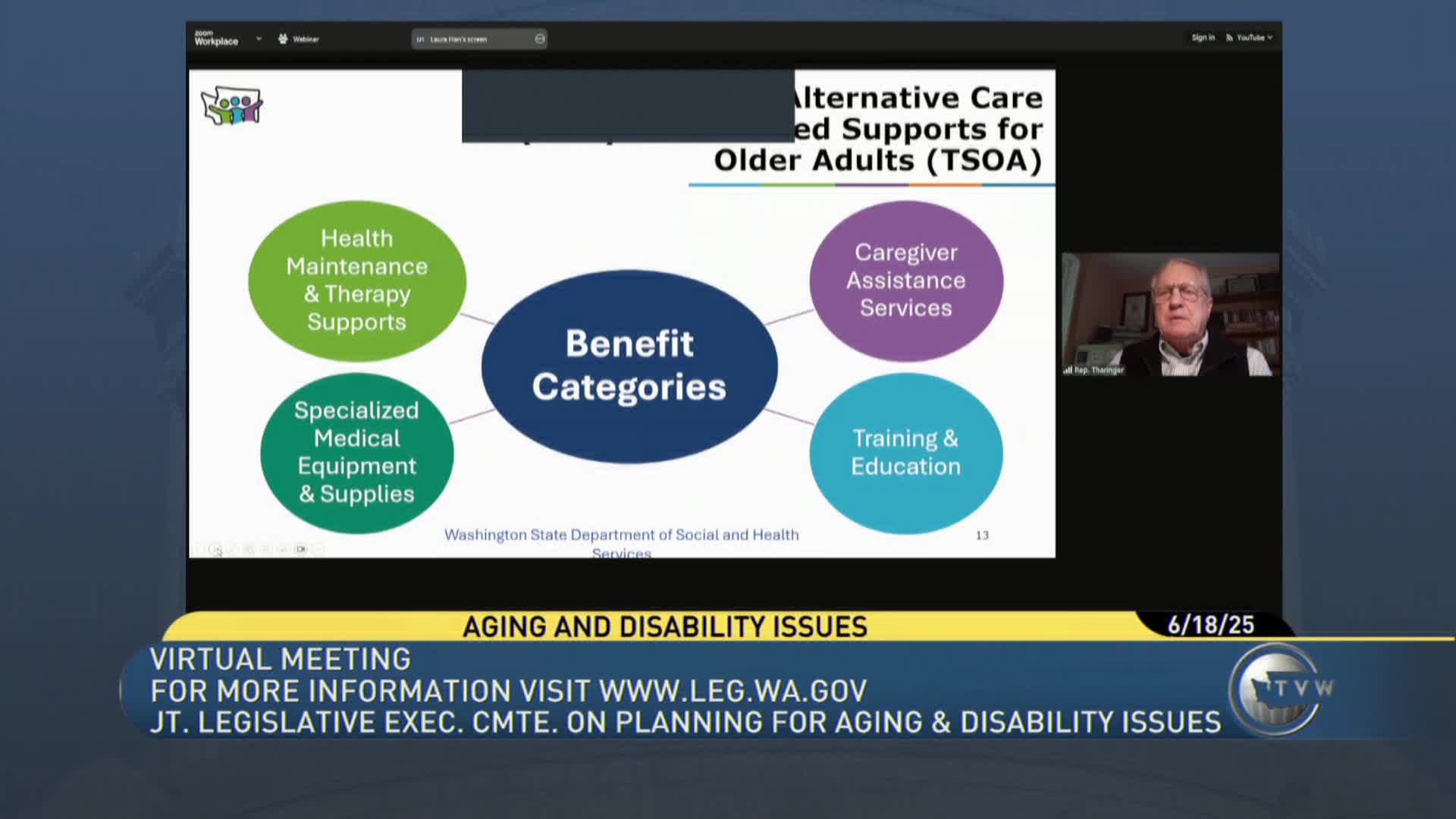
Summary
DSHS briefed JLAC on services added under Washington’s Medicaid 1115 ("11‑15") demonstration waiver, including caregiver supports, presumptive eligibility pilots and health‑related social needs benefits such as short‑term rental assistance.
The Department of Social and Health Services summarized components of Washington’s Medicaid 1115 demonstration waiver that expand long‑term services and supports, speed access to services and add health‑related social needs benefits.
Kathy Kinnaman, Director of Homeless Community Services at DSHS, described two waiver‑funded programs that target people not yet eligible for full Medicaid: Medicaid Alternative Care (MAC) and Tailored Supports for Older Adults (TSOA). Kinnaman said both programs “target pre‑Medicaid clients by supporting unpaid family caregivers and their care recipients” and use non‑general‑fund dollars matched by federal Medicaid payments.
Why it matters: DSHS said supporting unpaid caregivers is less expensive than institutional care and can delay Medicaid spend‑down. Kinnaman showed 2024 data comparing average monthly spending: about $600 per month in the unpaid family caregiver program versus roughly $4,600 per month for in‑home community residential care and nearly $11,000 per month for nursing‑home care. She said the unpaid caregiver benefit can help a person avoid spending down to Medicaid asset limits.
Key operational changes: The waiver also authorized presumptive eligibility, which lets certain clients receive a limited package of services quickly after an abbreviated assessment and then submit a Washington Apple Health application within 10 days. Phase 1 (December 2023) targeted people discharging from acute and community psychiatric hospitals; Phase 2 testing for statewide in‑home eligibility began in October 2024 in Region 1 with a planned statewide rollout in fall 2025. DSHS reported about 72% of presumptive applicants are found eligible and about 85% of those go on to traditional services.
Health‑related social needs (HRSN): The 1115 renewal that CMS approved in June 2023 added HRSN benefits DSHS can now bill under Medicaid—examples include rental assistance for up to six months, nutrition support, home modification and caregiver respite. DSHS said CMS approved protocols and rate methodology in January 2025, enabling initial implementation and pilots with Area Agencies on Aging.
Discussion vs. decisions: Committee members asked whether federal budget moves could jeopardize the waiver; DSHS said the existing waiver is likely secure until renewal (currently scheduled for 2028). Committee staff requested more granular data on how many people had been served under Phase 1; DSHS said it will provide that information after the meeting.
Ending note: DSHS told the committee it is piloting new processes and working with AAAs and managed‑care organizations to expand timely access to community supports and to use rental assistance to keep people housed and delay costlier institutional care.
