Utah Supreme Court weighs whether insurer discounts can reduce personal-injury awards
Get AI-powered insights, summaries, and transcripts
Subscribe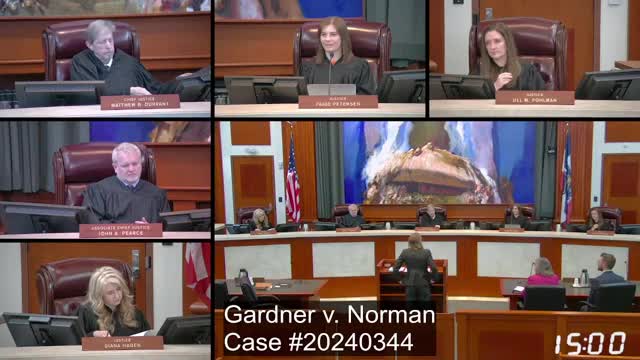
Summary
At oral argument, defense and plaintiff lawyers debated whether the collateral source rule bars use of insurer-negotiated discounts to lower medical damages and whether juries may see chargemaster (billed) rates or only amounts actually paid.
The Utah Supreme Court heard argument in a case arising from a personal-injury suit in which the parties dispute whether insurer-negotiated discounts to billed hospital prices can be used to reduce a plaintiff’s medical-damage award.
At the outset of the argument, Samantha Slark, counsel for defendant Tyler Norman, told the court that “these are not amounts that are paid by a collateral source,” and urged the justices to hold that the common-law collateral source rule does not apply to contractual discounts or write‑offs from billed (chargemaster) prices.
Slark framed two core points: (1) discounts or negotiated reductions are not payments by a collateral source, and (2) only amounts actually charged to and paid by a plaintiff or a collateral source should be admissible in proving medical damages. She said federal rules requiring hospitals to publish list prices show providers also publish cash and negotiated rates, and that in the case record the provider’s website reflects different prices for cash payors and third‑party payors.
Counsel for the appellee, Kara Porter, urged the court to preserve the collateral source rule’s traditional protection. Porter argued the rule prevents tortfeasors from benefiting when an injured person receives a reduction or other benefit “that was not procured by the tortfeasor,” and she cited Mahana and other authorities the court has previously relied on to show the rule’s scope. Porter warned that admitting evidence of amounts paid could require witnesses and testimony about insurer negotiations and internal billing practices, creating practical complications at trial.
Both sides identified a range of approaches adopted by other jurisdictions. Slark described three models: (1) allow only billed (chargemaster) rates at trial (an approach she called incorrect), (2) allow only amounts actually paid, or (3) admit both billed and paid amounts and let the jury determine reasonable value. She advocated the second model, saying the ceiling on recovery should be the amount actually paid, consistent with compensatory principles and the Restatement discussion cited in her filings.
Porter and several justices raised policy and practical questions the court would face whichever rule it adopts. Justices asked whether plaintiff-paid premiums or the plaintiff’s efforts to obtain discounts should affect recoverable damages, whether post‑verdict adjustments would be workable, and how the court should balance juror prejudice against the defendant’s right to present evidence about actual amounts paid. Counsel and justices also discussed the special statutory rules that apply to medical‑malpractice subrogation and to certain no‑fault payments (for example, argument noted that Personal Injury Protection, or PIP, payments were handled differently in the trial record).
Counsel agreed on one practical consequence: if the court concludes the collateral source rule does not bar evidence of discounts and that the amounts actually paid must be proved, the case record as it exists (in which evidence of amounts actually paid was excluded) could require further proceedings. Slark said that outcome likely would produce either a stipulation about amounts paid or a new trial so both sides could present comparable evidence.
The court heard extensive questioning about how hospital list prices are set, academic literature and state supreme‑court decisions such as Howell (California), and whether admitting paid amounts would unfairly reveal that an insurer rather than the plaintiff paid medical bills. Slark argued the discount benefits accrue to insurers or payors negotiating rates, not to plaintiffs themselves, citing other courts’ analyses that negotiate reductions are commercial arrangements between provider and payor.
After roughly an hour of argument and questions from the justices, the court recessed and put the case under advisement. The justices did not indicate a ruling timetable during argument.
