Patients, Cancer and Arthritis Groups Urge Ban on Copay Accumulator Adjustments
Get AI-powered insights, summaries, and transcripts
Subscribe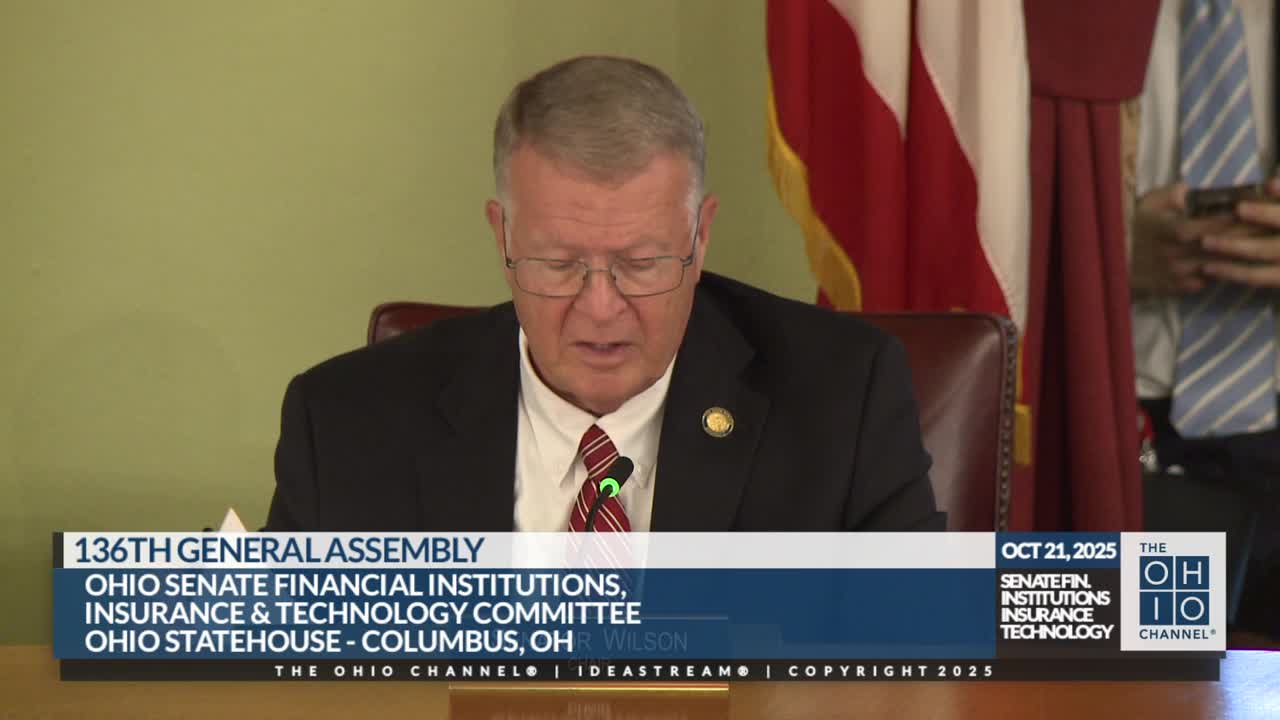
Summary
Patient advocates, the Arthritis Foundation, the American Cancer Society Cancer Action Network and other witnesses urged the Senate committee to pass Senate Bill 207 to ban copay accumulator adjustment programs and protect manufacturer and charitable assistance from being excluded from deductibles and out-of-pocket maximums.
Multiple patients and health advocates testified in favor of Senate Bill 207, which would ban copay accumulator adjustment programs and prohibit insurers and PBMs from excluding the value of manufacturer co-pay assistance and charitable patient-assistance payments from a patient's deductible and out-of-pocket maximum.
Kelly Chellis, a volunteer advocate for the Arthritis Foundation, told the committee her family relied on manufacturer co-pay assistance to obtain biologic medication for her daughter. "Senate Bill 207 would fix this by ensuring that when co pay assistance is used, it counts towards a patient's deductible and out of pocket maximum just as it should," Chellis said. She described a 2022 change in her insurer's plan that left her family paying thousands of dollars after the plan stopped counting assistance toward the deductible.
Amanda Vaught, another Arthritis Foundation volunteer living with ankylosing spondylitis, said manufacturer assistance is the only reason she could afford biologics and described the financial strain when assistance does not count toward cost-sharing. "Allowing co pay accumulators to count co pay assistance towards a patient's deductible and out of pocket maximum would provide the financial assistance that patients like me desperately need," she testified.
Leal Maida, Ohio relations director for the American Cancer Society Cancer Action Network, said co-pay assistance and charitable programs can be lifesaving for patients who lack generic alternatives and face high monthly drug costs. He cited a 2022 ACS CAN survey showing some cancer patients reported that assistance they received was not applied to deductible or out-of-pocket limits. Maida also raised concerns about "maximizers" and alternative funding programs run by PBMs that can remove drugs from coverage or shift patients into programs that deplete assistance without counting toward statutory out-of-pocket protections.
Witnesses asked the committee to advance Senate Bill 207 to protect patients from unexpected bills and preserve access to life-saving therapies. The committee took proponent testimony, reviewed multiple written submissions on members' iPads and adjourned; no vote on the bill was recorded in the hearing.
