Senate committee hears bill to require AI transparency in health-insurance prior authorization
Get AI-powered insights, summaries, and transcripts
Subscribe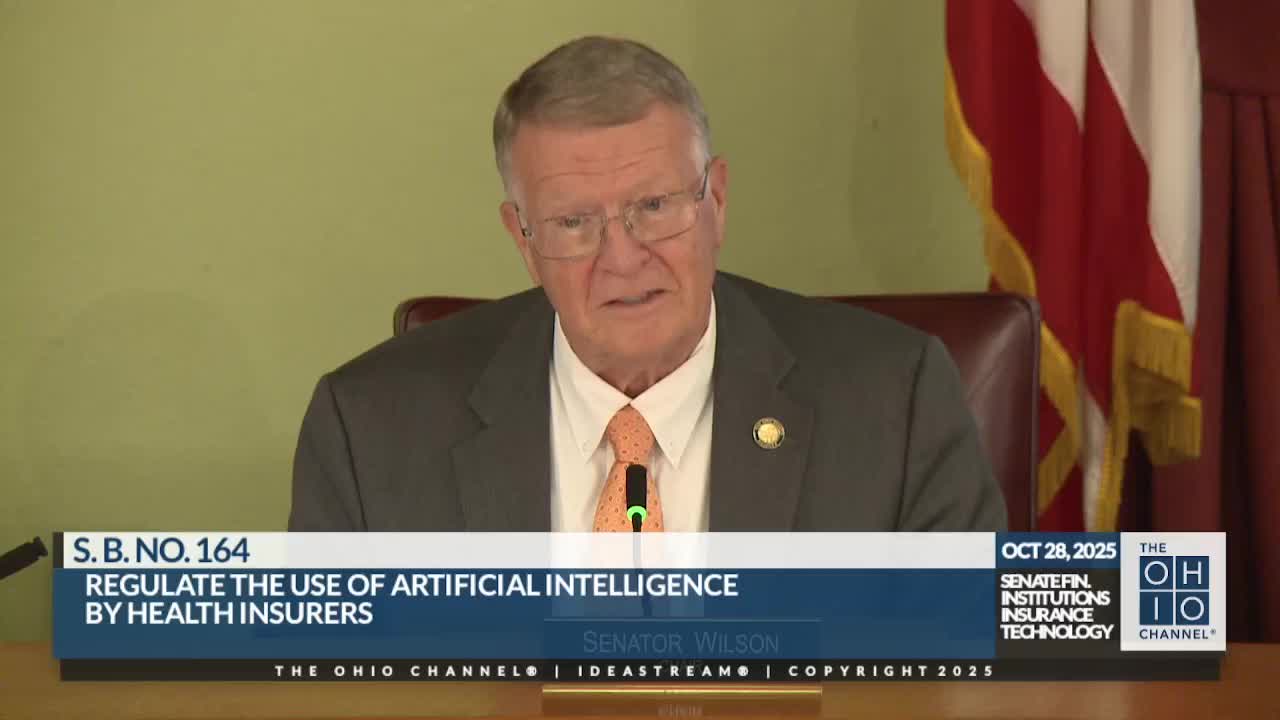
Summary
Sen. Catrona presented Senate Bill 164 to the Financial Institutions Insurance Technology Committee, proposing transparency and human oversight requirements for AI used in health-insurance prior authorization. Committee members asked about penalties and implementation; the measure received a first hearing and no vote.
Senator Mark Catrona on behalf of the sponsor told the Financial Institutions Insurance Technology Committee that Senate Bill 164 would require greater transparency and human oversight when insurers use artificial intelligence in health-care prior-authorization decisions.
Catrona said the bill would require disclosure of the algorithms, the criteria and the software used to make prior-authorization determinations and would ensure a human review layer. "Our overreliance of AI has triggered a multitude of denials...this bill is a transparency bill that provides a smooth, health care process," he said.
The bill, Catrona added, is motivated by what he described as an uptick in automated denials and by a November 2024 consensus statement from the National Association of Insurance Commissioners that encouraged states to pass transparency laws for AI in health care. "They themselves ... concluded that the rapid increase of AI usage in health care requires additional regulation to ensure that the consumers are protected," Catrona said.
Committee members noted the proposal focuses on transparency and oversight rather than specific penalties. Senator Blessing asked, "What's the penalty?" Catrona replied that the bill as introduced does not specify financial fines and that enforcement details could be considered during committee work. Senator Patz praised the human-review element, saying it helps clinicians catch issues that automated systems may miss.
The Financial Institutions Insurance Technology Committee held a first hearing on SB 164; no committee vote was taken and no amendments were adopted during the session. Further drafting and discussion were left to the committee record.
