HHS, FDA announce draft guidance to speed biosimilars, push interchangeability to lower drug costs
Get AI-powered insights, summaries, and transcripts
Subscribe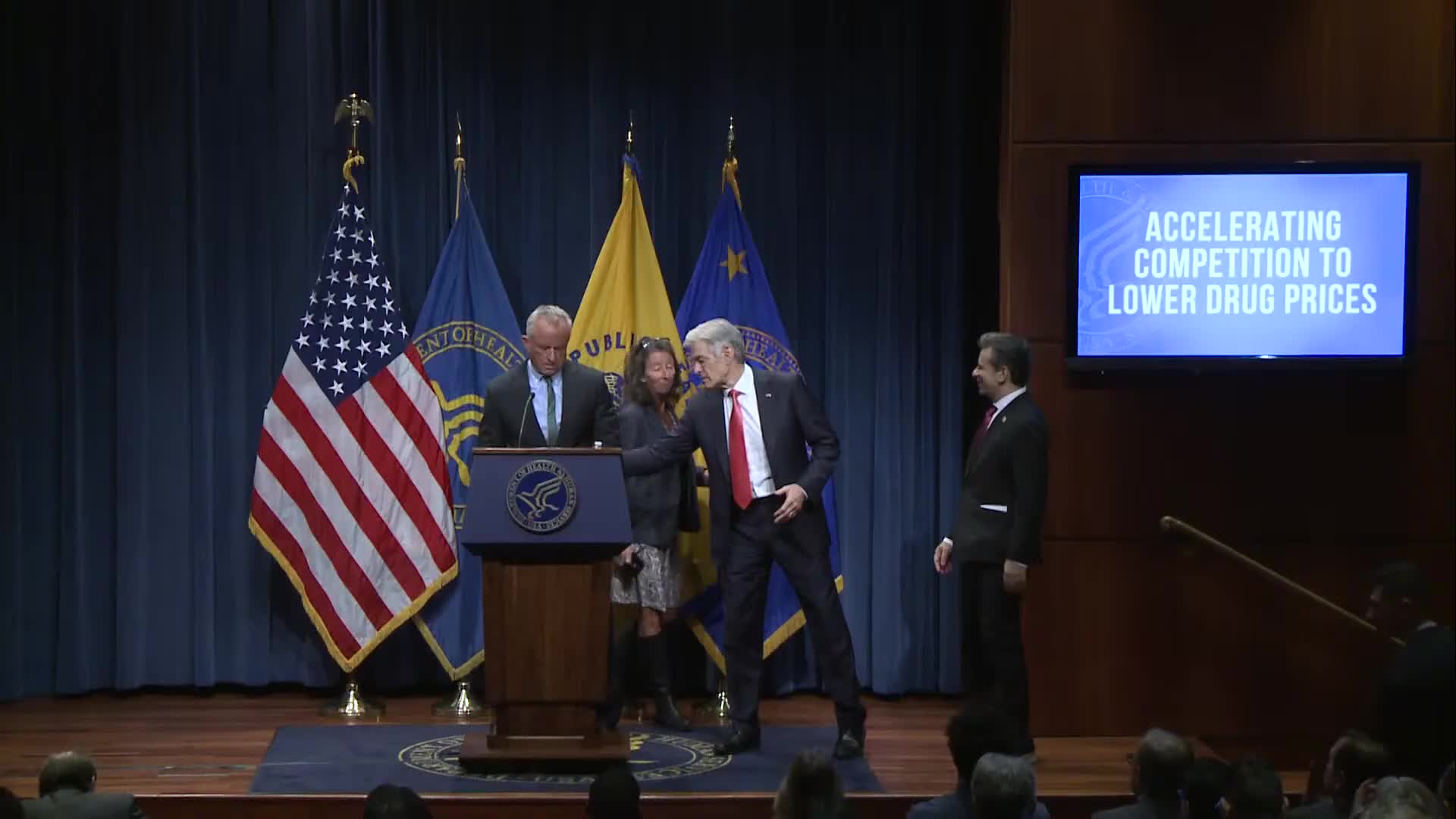
Summary
HHS Secretary Robert F. Kennedy Jr. and Food and Drug Administration Commissioner Marty McCary announced a package of FDA actions to streamline biosimilar approvals and promote interchangeability, steps officials said will shorten development times, cut industry costs, and increase competition to lower drug prices.
HHS Secretary Robert F. Kennedy Jr. and Food and Drug Administration Commissioner Marty McCary announced at a department briefing that the FDA will release draft guidance to streamline the approval pathway for biosimilar medicines and to promote interchangeability with reference biologic drugs. Officials said the steps are designed to shorten development timelines, lower industry costs, and increase competition to bring down prices for patients and federal payers.
Kennedy said the current system has allowed monopolies to persist after patents expire and that regulatory and contractual barriers have slowed biosimilar entry. "This is not acceptable in the United States of America," Kennedy said, framing biosimilars as a central lever to reduce outlays for expensive biologic medicines.
The nut of the announcement is twofold. First, FDA will issue draft guidance making clear when advanced analytical testing can replace large, expensive human comparative trials for many biosimilar applications. Second, the agency will consolidate multiple outdated guidance documents into a single, streamlined framework and take a more expansive view of interchangeability so pharmacists can substitute biosimilars in more cases.
"Under this new framework, companies may not always need to conduct large expensive human trials when advanced testing can already prove that biosimilars work just as effectively and just as safely as the original drug," McCary said. He told reporters the changes could shorten the typical biosimilar development and approval timeline from roughly five to eight years to about two and a half to five years and save companies "about a $100,000,000 in their development cost," figures officials attributed to industry estimates shared with the agency.
Officials cited the scale of the issue: biologic medicines make up only about 5% of prescriptions but account for a majority of drug spending, with U.S. spending on biologics rising from roughly $100 billion in 2013 to $260 billion in 2021 and to about $407 billion by 2024, according to figures Kennedy offered at the briefing. FDA Commissioner McCary said biosimilars have already generated roughly $56 billion in savings since 2015 and about $20 billion in 2024 alone.
McCary said the agency will also take steps to increase the number of biosimilars designated as "interchangeable," eliminating the routine requirement for switching studies used in some previous determinations. "We're saying basically we think all biosimilars should be interchangeable," he said, while noting that state laws control whether pharmacist substitution requires patient consent.
When asked for a timeline, McCary said FDA expects to issue final interchangeability guidance in roughly three to six months. He added the agency will publish clearer, consolidated rules to provide predictability for investors and manufacturers.
Officials pointed to market examples to explain the policy goals. Reporters cited Humira, a high-volume biologic for which multiple biosimilars eventually entered the market but did not immediately displace the brand. McCary and other officials said formulary contracting practices involving pharmacy benefit managers (PBMs) and lack of pricing transparency can blunt biosimilar uptake; the administration asked for greater transparency and highlighted voluntary PBM changes and a pricing-publishing tool called "Trump Rx" to surface actual medication prices.
Dr. Mehmet Oz, speaking for Centers for Medicare & Medicaid Services (CMS) interests at the briefing, urged patients to ask clinicians about lower-cost biosimilar options, asked insurers to design plans that do not disincentivize biosimilar use, and told governors to prepare to capture Medicaid savings. "When you get a paycheck, there's a deduction for a Medicare excise tax. All of that money is getting routed towards these expensive biologics," Oz said, urging insurers and state programs to take advantage of the lower-cost alternatives the agencies expect to encourage.
Officials said the reforms will have implications across pharmacies, PBMs, hospitals, and federal programs (Medicare and Medicaid) and emphasized that the agency will solicit public comment on draft guidance before finalizing rules. Commissioner McCary characterized the changes as administrative actions the FDA can take without waiting for new legislation, while acknowledging congressional action could further solidify interchangeability in law.
The briefing included questions about other topics. Kennedy said the administration is "looking at the feasibility" of separating the measles-mumps-rubella (MMR) vaccine into separate shots at the president's request and described the evidence linking prenatal acetaminophen (Tylenol) use to neurodevelopmental outcomes as "suggestive" but not definitive, advising pregnant patients to consult their physicians. On the Affordable Care Act marketplace, speakers disputed a specific claim about premium increases and said decisions about extending COVID-era tax credits rest with Congress.
Next steps: FDA will publish the draft guidance for public comment, with McCary projecting a final interchangeability guidance in about three to six months. CMS encouraged insurers and state Medicaid programs to consider benefit and procurement changes that would make low-cost biosimilars more accessible to patients.
Context and limits: Officials repeatedly framed these moves as administrative and regulatory changes rather than statutory reforms; McCary noted state substitution laws and possible legal challenges could affect how interchangeability and substitution play out in practice. The agencies provided numerical estimates for savings and timelines that they described as informed by industry and agency analysis; officials did not provide an exhaustive, auditable calculation in the briefing.
