Health systems and clinicians tell House panel telehealth, remote monitoring and value-based models lower costs and hospitalizations
Get AI-powered insights, summaries, and transcripts
Subscribe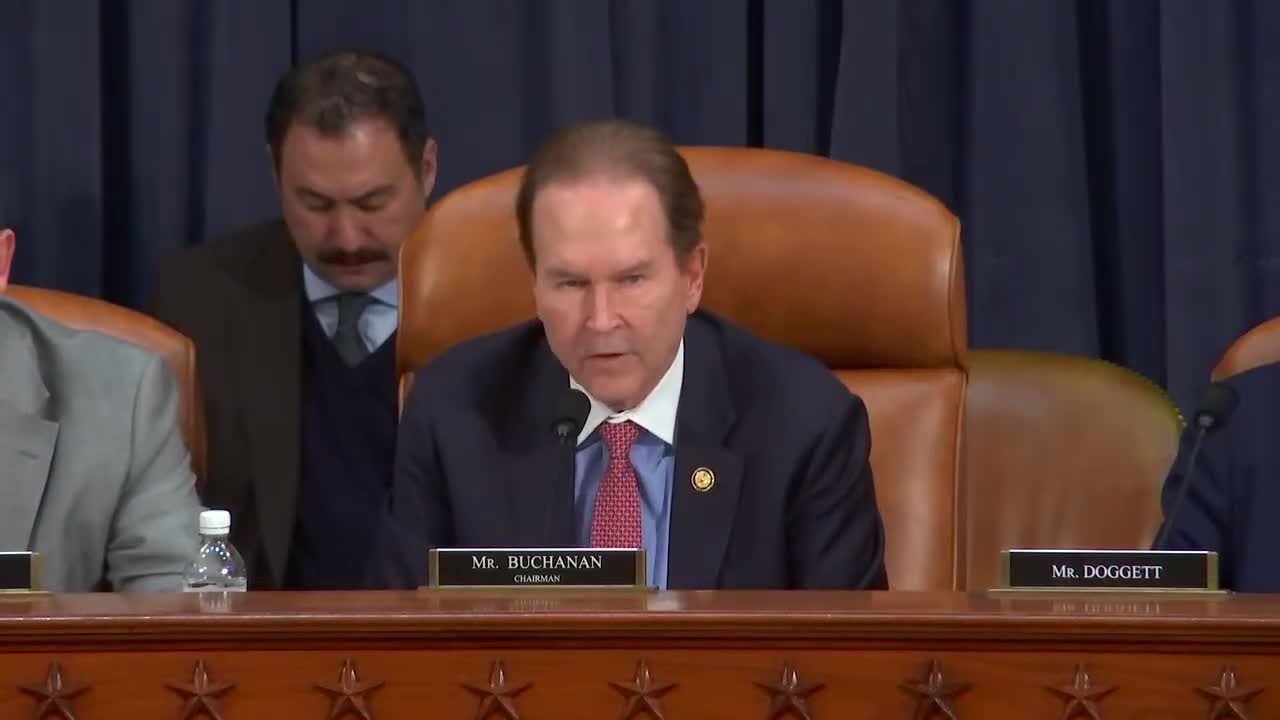
Summary
Hospital systems and physician groups told the subcommittee that telehealth, remote patient monitoring and accountable-care/value-based payment models can improve prevention and chronic-disease outcomes while reducing hospital and ER use; witnesses cited ACO savings and program results.
WASHINGTON — Providers and health-system leaders told a House Ways and Means subcommittee that combining telehealth, remote patient monitoring and value-based payment models can improve chronic-disease outcomes while bending the cost curve.
Dr. Michael Hoban, chief medical officer for population health services at Novant Health, described the systems integrated care teams and said Novant's ACOs have saved "over $90,000,000 net since 2017" while maintaining high-quality rankings. Hoban pointed to telehealth numbers and programs — including telestroke, hospital-at-home and community paramedics — as evidence that remote tools can reduce time to care and prevent hospitalizations.
Dr. Ashish Parikh, a primary-care physician and chief population health officer at Summit Health, told the committee a single case in his clinic illustrated coordinated care: through a virtual behavioral-health consult, a patient with suicidal thoughts was safely kept at home with close follow-up, avoiding an emergency-room visit and hospitalization. Parikh said unstable reimbursement and misaligned incentives remain the primary barriers to investing in the social and clinical infrastructure needed for team-based care.
Both witnesses described alternative payment models as a practical route to enable investments in care management. Parikh and Hoban said that when groups participate in shared-savings ACO programs and are held to quality metrics, they can invest in nurse care managers, community health workers and pharmacy collaboration that reduce readmissions and emergency visits.
Committee members asked about older adults and rural residents. Witnesses recommended making pandemic-era telehealth flexibilities permanent, expanding remote monitoring and simplifying telehealth access for seniors (including audio-only options and one-click links). The hearing produced no formal votes; members left the record open for written follow-ups.
