Kansas agency to switch IDD waiver eligibility tool to MFEI March 1, 2025; KDADS says current services protected
Get AI-powered insights, summaries, and transcripts
Subscribe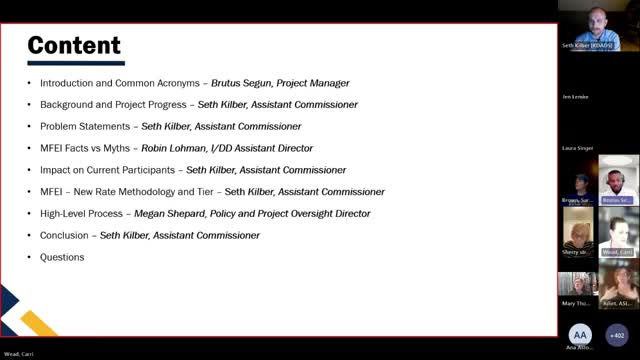
Summary
KDADS announced it will replace the BASIS assessment with the Medicaid Functional Eligibility Instrument (MFEI) for IDD waivers on March 1, 2025, with existing participants’ reimbursement tiers held until at least July 1, 2026, and ARPA‑era reassessments using BASIS if needed to prevent loss of services.
KDADS announced that it will begin using the Medicaid Functional Eligibility Instrument (MFEI) to determine functional eligibility for intellectual and developmental disability (IDD) waivers starting March 1, 2025.
Seth Cuber, assistant commissioner for long‑term services and supports at the Kansas Department for Aging and Disability Services (KDADS), said the shift is intended to replace the decades‑old BASIS assessment with a more standardized, strengths‑based tool that better aligns with the NRI suite of assessment instruments and addresses inconsistencies that have drawn federal scrutiny. "We need to stand up a level of care tool that will allow for a lot more freedom and flexibility for waiver participants," Cuber said.
KDADS officials told participants that existing waiver recipients will be reassessed using the MFEI beginning March 1, but their reimbursement tiers will not be adjusted until at least July 1, 2026, to give the state and stakeholders time for a rate study and transition. "You will not lose any services," Cuber said when asked about the risk of service loss during the changeover.
Robin Lohman, assistant IDD director, ran a "myths vs. facts" segment and confirmed several operational details: the MFEI go‑live date is March 1, 2025; providers and targeted case managers already are required to maintain medical documentation; and the MFEI determines functional eligibility (eligible vs. not eligible) but does not itself assign tiered reimbursement rates. "The MFEI IDD only determines functional eligibility," Lohman said. She added that while assessment questions and responses can be requested, the private scoring algorithm will not be publicly available.
KDADS said the new approach is data driven and intended to be budget‑neutral. Cuber said rates will be informed by multiple validated data sources — the MFEI level‑of‑care evaluation, NRI service‑planning data collected by managed care organizations (MCOs), and other evaluation scales — and that a rate study is planned for early 2025 to support future rate setting. Officials described a simplified rate framework of three standard rates plus a complex‑needs rate, replacing the current 10‑tier BASIS structure.
To ease concerns about short‑term fluctuations in behavior data, KDADS said it will preserve appeal rights and will assign KDADS IDD staff to perform a follow‑up BASIS assessment for anyone found ineligible under the MFEI during the American Rescue Plan Act (ARPA) maintenance‑of‑effort period that runs through the end of 2025. "If an individual were to be determined ineligible using the MFEI, the BASIS would be used to do a reassessment," Lohman said.
Presenters acknowledged stakeholders' concerns about MCOs' role in needs‑evaluations and potential conflicts of interest when MCOs contribute to tier determinations. A caller labeled "provider (unverified)" asked whether MCOs would have undue leverage when assigning rates; Cuber replied that KDADS will increase oversight and scaffold the MCO process to meet CMS expectations for state involvement.
KDADS said materials and supports will be available to stakeholders: the MFEI instrument will be distributed after the webinar, an adapted Kansas MFEI‑IDD manual will be released, KDADS will publish FAQs and short explanatory videos, and the agency plans open hours and additional meetings (scheduled Jan. 21 and Feb. 18) to answer questions ahead of March 1.
Stakeholders on the call urged clearer communication about how tier labels will be presented to families; KDADS acknowledged that labeling conventions are changing and promised to emphasize clarity to avoid confusion as the new tiers are implemented.
The department encouraged questions via a project email and its IDD modernization website and said it would continue stakeholder engagement as rate work and implementation proceed. The webinar closed with staff reiterating contact information and upcoming outreach opportunities.
