HCPF outlines soft caps, 56‑hour caregiver limit and fast rule timeline for Community First Choice services
Get AI-powered insights, summaries, and transcripts
Subscribe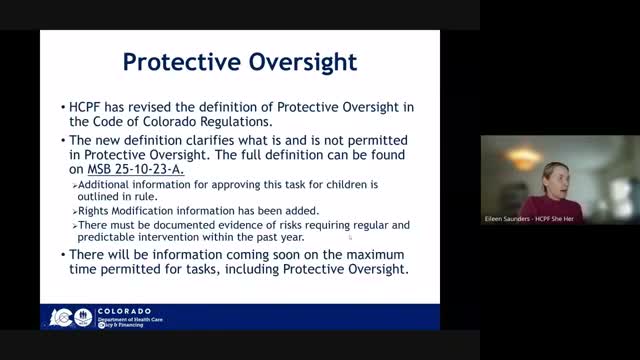
Summary
Colorado’s Health Care Policy & Financing department announced annual ‘soft caps’ on Community First Choice services and a 56‑hour per‑week, per‑caregiver limit, to be implemented via emergency rules in mid‑February with permanent rules next spring; stakeholders warned of access risks and appeals.
The Colorado Department of Health Care Policy and Financing (HCPF) told its Community First Choice (CFC) Council in December that it will implement several sustainability measures in 2026 that limit units and caregiver hours for CFC services while preserving an exceptions process.
Lana Eggers, who leads waiver and CSC-related work at HCPF, said the governor’s October budget to close a multimillion-dollar shortfall requires cost‑saving steps across state agencies and prompted the changes. HCPF announced annual "soft caps" of 10,000 units per year for personal care, 4,500 units per year for homemaker services, and 19,000 units per year for health maintenance activities. The department said those caps are ‘‘soft’’—case managers may request exceptions and the department will approve additional units when a member’s assessed needs warrant them.
Eggers also announced a 56‑hour weekly cap per caregiver for a single member that applies across multiple services (personal care, homemaker, health maintenance activities, long‑term home health and related nursing services). HCPF emphasized that the existing 16‑hour‑per‑day individual caregiver limit remains in place for safety, and that hours above the 56‑hour cap must be staffed by a secondary caregiver rather than by extending a single caregiver’s week.
The department said it will reduce the weekly homemaker limit when provided by a legally responsible person from 10 hours to 5 hours; members who need more homemaker hours may still receive them if another, non‑legally responsible caregiver provides the additional hours.
HCPF said the policy changes are tied to an executive order and budget decisions and that the limits themselves were set in the governor’s budget; the department is proposing rule language to clarify definitions, caregiver limits and service limits and to add an age‑appropriate task‑standards definition for children.
To allow case managers time to prepare, HCPF will run emergency rules to be considered by the Medical Services Board in mid‑February and effective in mid‑February, with permanent rulemaking to follow beginning in April and an anticipated permanent effective date in May. HCPF plans to post a stakeholder rule draft in mid‑December and accept public feedback for about a month, with comments due around Jan. 12.
Officials reiterated that exceptions processes will exist. Kidron (HCPF legal staff) said the department expects denials through service planning to trigger a notice of action and an appeal right following existing waiver appeal pathways; HCPF said it will coordinate with its legal division and the attorney general’s office to refine guidance.
Stakeholders at the meeting urged the department to reconsider or clarify the changes. Molly, a former Clear Creek County case manager, said the 56‑hour cap risks ‘‘kneecapping’’ an already strained workforce and could leave members partially served or push families toward institutional care. Tara of About Kids Home Care asked why the state would pay up to 112 hours in total but cap a single caregiver at 56 hours, calling the situation hard to explain to families. Lauren warned the cap may cause rural households to lose access to sufficient caregivers and could unintentionally increase nursing‑home placements and program costs.
HCPF said it will publish operational guidance, the updated Direct Care Services calculator and a memo explaining the task standards and appeals process. The department directed stakeholders to its Medicaid sustainability website, the OCL newsletter and stakeholder engagement pages for the rule draft, listening sessions and comment instructions.
The department did not adopt the final limits during the council meeting; instead it announced the planned caps, the exceptions and appeal pathways, and the emergency‑rule timetable that will determine when new case‑management authority and operational changes take effect.
