Committee hears insurance, staffing and risk updates after new Illinois drug-fee law
Get AI-powered insights, summaries, and transcripts
Subscribe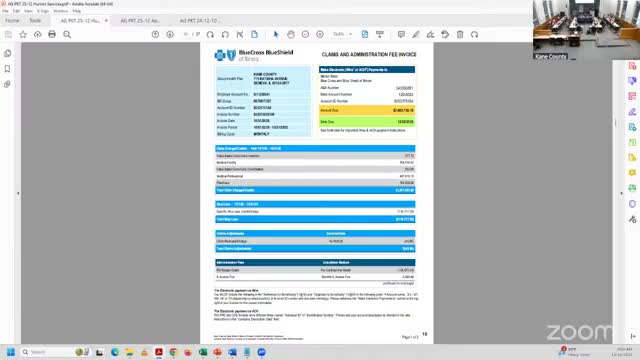
Summary
Staff reported a new Illinois Prescription Drug Affordability Act fee that will add about $15 per participant per year (implemented by carriers as roughly $1.25/month) to the county's health insurance fund to finance grants to community pharmacies; members also raised dental plan concerns and received risk, staffing and training updates.
At a Kane County Human Services Committee meeting, staff briefed members on a new Illinois Prescription Drug Affordability Act fee, ongoing staffing and training reports, and winter risk management updates.
Jamie Libero, staff, told the committee that two bills referenced in the transcript (identified as "house bill 16 97" and "house bill 7 67") establish a $15-per-employee-per-year charge tied to prescription drug coverage to fund grant dollars for community pharmacies. Libero said the law will seed roughly $25,000,000 in grants to community pharmacies and that the charge will be taken out of the county's health insurance fund, which could affect future rates. "So it'll come out of the health insurance fund," Libero said, adding that Blue Cross will incorporate the charge monthly on billing at about $1.25 per month and then pay the annual fee on the county's behalf.
Committee members asked who qualifies as a "community pharmacy"; Libero said she did not have the definition on hand and offered to research and report back to the committee.
David Larson, the county's risk manager, reported a relatively mild winter so far, initial site visits completed, and that departments had been responsive to requests. Libero also described planned changes to staffing reports so the committee sees a complete monthly picture and summarized training compliance, noting high participation and a possible no-cost training video from the Illinois Department of Human Rights.
A committee member raised concerns about dental insurance claim payments and coverage limits such as counts for cleanings and exams; Libero explained the county is fully insured for dental with Cigna, which the county selected for network breadth and competitive cost, and offered to price higher-benefit plans and investigate specific claim issues. "If someone has a lot of dental work, there is a lot left to be desired on it," Libero said, acknowledging limitations typical of dental coverage.
Reports were placed on file by unanimous consent after Miss Allen moved to do so. The meeting concluded with a motion to adjourn.
Staff agreed to research the definition of "community pharmacy," provide additional benefit-plan pricing if requested, and follow up on specific dental claim concerns.
