Lawmakers discuss residential substance‑use treatment coverage and recovery bill planning
Get AI-powered insights, summaries, and transcripts
Subscribe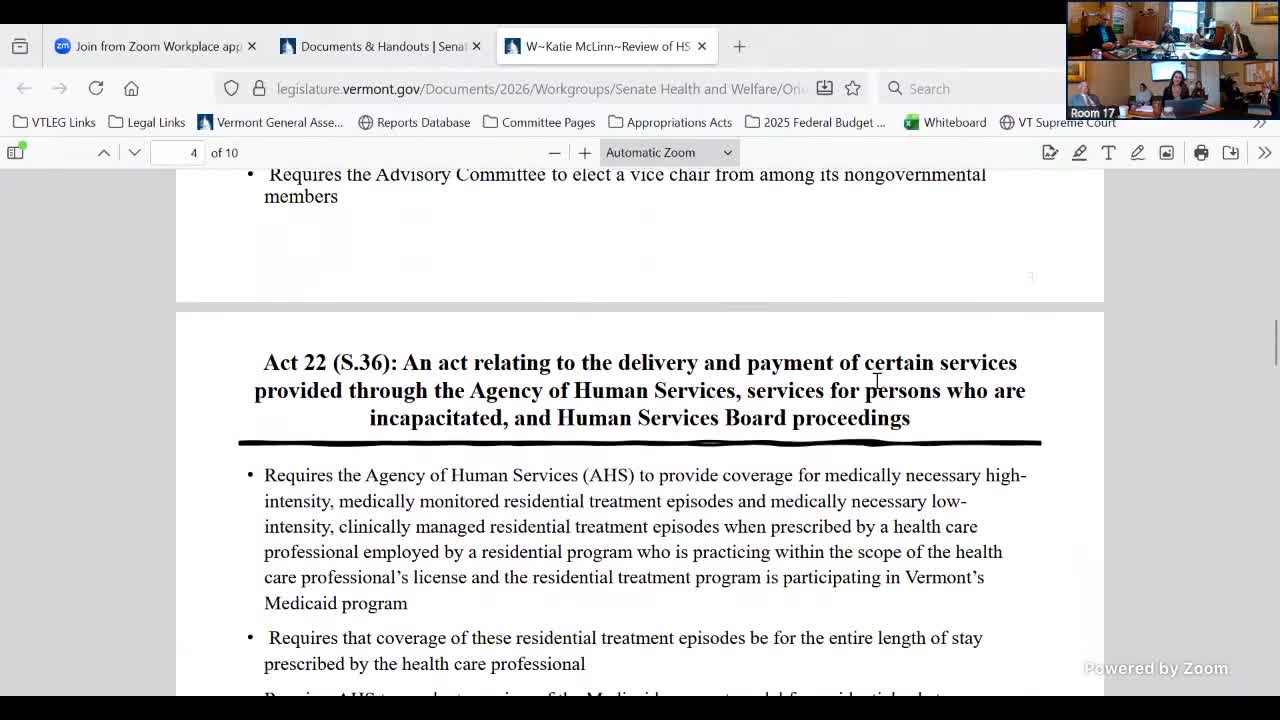
Summary
The committee reviewed provisions from Act 22 (S36) requiring AHS to cover medically necessary, medically monitored residential treatment and to review Medicaid payment models; members also discussed the repeal of old 'public inebriate' language and planned presentations from Health, DMH and DOC on services for incapacitated individuals.
The Senate Health & Welfare committee examined Act 22 (S36) and related recovery work. Speaker 2 summarized the bill's residential‑treatment language and said it requires AHS to provide coverage for “medically necessary, high intensity, medically monitored residential treatment episodes” and for clinically managed lower‑intensity residential episodes when prescribed by a licensed health professional and when the program participates in Medicaid.
Speaker 2 said the act requires AHS to conduct a review of the Medicaid payment model for residential substance‑use disorder treatment and to submit that review to the General Assembly and LEHI. Speaker 1 recommended the committee review that payment‑model report before taking up the recovery bill (S157).
Separately, Speaker 2 explained the bill repealed older statutory language often referred to colloquially as 'public inebriate' and clarified the statute refers to "persons who are incapacitated" due to alcohol or other drugs. The change removed the earlier prohibition that would have prevented holding incapacitated persons at DOC facilities; the statute now requires DMH and Health to expand services and programming for that population, prioritize Chittenden County and deliver presentations to the General Assembly.
Next steps: the committee plans to schedule the AHS/DMH/DOC presentations and review the payment‑model report before moving forward with the recovery bill.
