AHS tells House Appropriations HR 1 will shift Medicaid funding and reduce provider-tax revenue
Get AI-powered insights, summaries, and transcripts
Subscribe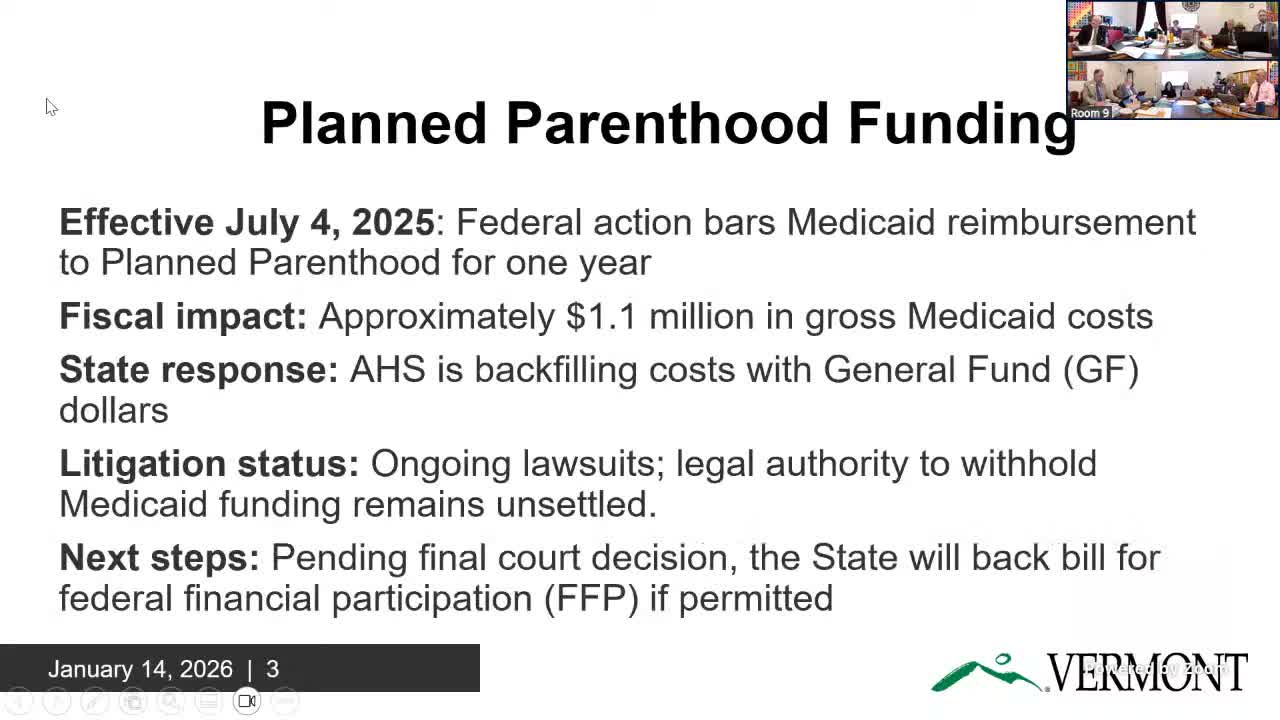
Summary
Agency of Human Services officials told the House Appropriations Committee that HR 1 will bar federal Medicaid reimbursements to Planned Parenthood for a year (the state will backfill with general fund), cap and step down provider taxes with multi‑year general‑fund impacts, limit state‑directed payments to Medicare rates, and require more CMS guidance before implementing cost‑sharing changes.
The House Appropriations Committee on Jan. 14 heard Agency of Human Services officials warn that HR 1, the federal budget reconciliation bill passed July 4, 2025, will materially change how Vermont pays for Medicaid and could reduce state revenues. Agency witnesses described an immediate one‑year prohibition on federal Medicaid reimbursements to Planned Parenthood, a multiyear step‑down of hospital provider taxes, new limits on state‑directed payments and a future requirement for expanded cost sharing.
"HR 1, which is the big, beautiful bill that was passed on 07/04/2025," said Ashley Berliner, director of Medicaid policy for the Agency of Human Services, as she outlined the law's main provisions for the committee. Berliner said the first provision to take effect barred Planned Parenthood and similar entities from receiving federal Medicaid reimbursement for one year and that the agency has chosen to "backfill all of the lost federal financial participation with state general fund." She told the committee AHS identified about $1,100,000 in gross Medicaid costs tied to Planned Parenthood in Vermont and that the state will cover about $600,000 of that cost for one year.
Berliner also described a set of changes to provider taxes. "Effective on the passage of this bill, there is a prohibition on the creation of any new provider taxes," she said, and starting November 2027 existing hospital provider‑tax caps must step down by 0.5 percentage point per year. AHS told the committee the step‑down will have immediate and growing general‑fund effects; agency staff summarized an initial impact of about $18 million in reduced general‑fund revenue and said the cumulative reduction over five years would amount to roughly $87 million.
Committee members sought clarity on mechanics and on whether provider‑tax receipts directly fund Medicaid. Berliner said provider‑tax revenue is deposited into the general fund and is not a direct, one‑for‑one match to Medicaid rates in Vermont, noting the relationship differs from other states that use provider taxes to flow funds directly back into provider rates.
On state‑directed payments (SDPs), Berliner said HR 1 treats SDPs as a distinct category and will prevent their inflationary growth. "Any new state‑directed payments must be capped at 100% of the Medicare rate," she said, and existing SDPs must be reduced by 10% per year starting in 2028 until they reach parity with Medicare. AHS said it will inventory legislative directives that instruct the Department of Vermont Health Access how to pay providers so the state can identify which payments fall under the SDP rules and seek ways to preserve policy priorities without triggering the caps.
The bill also includes a future requirement to expand Medicaid cost sharing for the new adult population. Berliner said the cost‑sharing provision takes effect in October 2028 and would require co‑payments beyond the limited set Vermont now uses; she emphasized that the agency is awaiting Centers for Medicare & Medicaid Services (CMS) rulemaking to clarify what is and is not permitted under the statute.
AHS repeatedly cautioned the committee that several provisions are subject to legal and regulatory change. On the Planned Parenthood restriction, Berliner said there has been ongoing litigation with injunctions and pauses and that AHS will "wait on a final court decision before making any changes." She said if a court overturns the restriction the state would seek to recoup federal claims.
Agency officials told the committee they are actively working to model budget impacts, consult attorneys and develop "guardrails" so the state can remain compliant while protecting policy goals. There were no committee votes; AHS said it will return with more detailed fiscal analysis, an inventory of SDPs and recommendations for legislative language to preserve program priorities.
What happens next: AHS will follow up with detailed budget projections, an SDP inventory and legal analysis; the committee will consider those materials as part of the FY27 budget process.
