DOC, Wellpath outline Medicaid reentry plans and operational fixes to improve continuity of care
Get AI-powered insights, summaries, and transcripts
Subscribe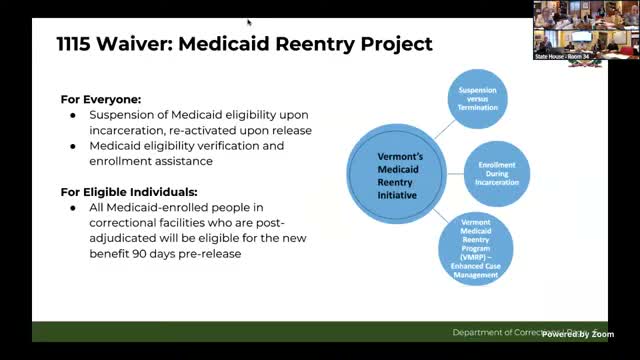
Summary
DOC and Wellpath told the House Corrections Committee the state will suspend (not terminate) Medicaid during incarceration, enroll eligible people while incarcerated, and stand up six reentry coordinators; they also described screening, staffing and technology fixes intended to reduce backlogs and improve continuity of care.
Department of Corrections and Wellpath officials described on Jan. 15 how new Medicaid policy changes and operational improvements aim to reduce gaps in care when people enter and leave custody.
Aviva Tabra (Vermont DOC) summarized the Medicaid reentry changes that will suspend, rather than terminate, Medicaid during incarceration and enable automatic reactivation on release. "That should happen within 24 hours," Tabra said of reactivation. The change, together with DOC/Wellpath screening and enrollment work, is intended to reduce coverage gaps at release and allow the state to bill Medicaid for some pre‑release services up to three months before a person’s release.
Tabra said the state will reinvest claim reimbursements into enhanced reentry supports through the Vermont Chronic Care Initiative (VCCI). The program will add six reentry care coordinators statewide, and Wellpath will expand nurse discharge planners at every site to improve release planning and continuity with community providers.
Presenters also described several operational and clinical topics the committee called out. Intake screening is completed by nursing at booking and a provider assessment (a physical exam by a nurse practitioner, PA or physician) is the goal within seven days; additional mental‑health and substance‑use assessments follow as indicated. Ginny Oliver, Wellpath’s medical director for Vermont DOC, told members the contract has supported clinical standardization, EHR redesign and continuous quality improvements that reduced backlogs: medical/dental past‑due appointments dropped by about 80% since last February and psychiatrist appointment backlogs fell by roughly 97% in the same interval.
Members raised specific concerns about continuity for transfers, treatment for people on methadone, translation and point‑of‑care testing. Oliver acknowledged some transfers arrive with incomplete medication information and said methadone continuity is a recurring challenge. She also said the system lacks point‑of‑care fentanyl urine testing: "We don't have fentanyl urine drug screening at point of care, that's a big problem," she said. Committee members pressed for better interpretation services and for technology fixes; presenters described CorrectTech connectivity problems that can drop remote EHR sessions on brief network blips and said those interruptions slow clinical workflow.
DOC and Wellpath committed to supplying additional slides and follow‑up details and to working with the committee and reentry partners (VCCI/BCCI) as the Medicaid rollout and reinvestment plans proceed. The committee said it will continue oversight in upcoming hearings.
